It was 1989, and she was still a resident anesthesiologist, Dr. Heidi Klessig recalled in her book, “The Brain Death Fallacy.”
One day, her attending anesthesiologist told her to prepare a brain-dead organ donor for organ removal surgery.
Upon examining the patient, Dr. Klessig was surprised to find that the man looked exactly like every other critically ill, living patient and, in fact, better than most.
Her answer was a paralyzing agent so the donor would not move during surgery, as well as some fentanyl to blunt the body’s responses to pain.
The anesthesiologist looked at her and asked, “Well, are you going to give anything to block consciousness?”

Dr. Klessig was stunned. Consciousness blockers are given to patients to ensure they are not awake and aware during an operation.
Her education told her that brain-dead patients should not be conscious; apart from having a biologically active body, their minds were gone.
“I looked at him and said, ‘Why would I do that? Isn’t he dead?’”
Her attending anesthesiologist looked at her, asking, “Why don’t you give him something to block consciousness—just in case.”
“I get a pit in my stomach every time I remember his face,” Dr. Klessig told The Epoch Times. “I remember him looking at me over his mask ... It seemed very confusing.
Is Brain Dead, Dead?
Once a person is brain dead, they become legally dead, but their bodies are technically still alive.The definition of brain death, also known as death by neurological criteria, is when a person falls into a permanent coma, loses their brainstem reflexes and consciousness, and cannot breathe without stimulus or support.
However, all of this stops if they get taken off life support.
For this reason, physicians hotly contest whether brain death is synonymous with death.
Dr. James Bernat, a neurologist and professor emeritus at the Dartmouth Geisel School of Medicine, told The Epoch Times that people who are brain dead are dead because their bodies “no longer function as an organism as a whole.” Without the technology to develop these life support machines, these people would be dead, he said.
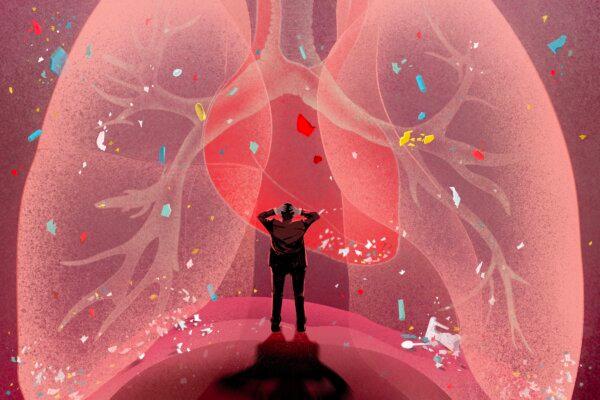
Another topic regarding brain death is whether a patient can still feel.
Among European anesthesiologists, there is an ongoing debate about whether brain-dead organ donors should be given consciousness blockers during organ procurement.
Mr. Miller, who is also a professor of medical ethics in medicine at Weill Cornell Medical College, said the label of brain death is misleading. He and Dr. Truog, professor of anesthesiology and director emeritus of the Harvard Medical School Center for Bioethics, are of the opinion that brain-dead people are alive but will likely not regain consciousness and recover.
Jahi would move to instructions, nurses and doctors testified. Later, an electroencephalogram (EEG) detected brain wave signals.

A brain-dead person should have no EEG activity whatsoever.
How Is Brain Death Assessed?
According to the most recent brain-death assessment guidelines, published by the American Academy of Neurology (AAN) in 2023, brain death is determined through a bedside assessment.Before the brain-death assessment is conducted, neuroimaging must be done to ensure there is damage to the brain.
“If you see a normal CAT scan or a normal MRI, then you need to be very, very careful and cognizant that you may be going to a false-positive situation,” Dr. Panayiotis Varelas, one of the co-authors of AAN’s 2010 guidelines and chair of the Department of Neurology at Albany Medical College, told The Epoch Times.
After brain injury is confirmed, two doctors then complete the brain-death assessment. The patient is tested twice for their responsiveness to pain stimulus and brainstem reflexes, with a 24-hour interval between each test.
If the patient tests positive both times, the doctors will conduct an apnea test—considered the most conclusive—to see if the person has lost breathing reflexes. In children, there are two apnea tests, one after each bedside brain-death assessment.

During the apnea test, the patient is taken off the ventilator for 10 minutes. A tube carrying pure oxygen is inserted into the airways. If the patient does not breathe voluntarily, they are considered brain dead.
The apnea test comes with several risks.
For example, those with respiratory failure may experience complications, including severe hypotension, hypoxia, and cardiac arrhythmia.
In a patient whose brain is already compromised, an apnea test may worsen the person’s condition or cause further damage, Dr. Paul Byrne, regarded as a pioneer in neonatology and involved in treating supposedly brain-dead neonates, told The Epoch Times. A worse condition can compound a brain-death diagnosis in individuals who may actually be on track for recovery.
Misdiagnosis could also occur during brain-death assessment.
One example is Zack Dunlap. In November 2007, he got into a traffic accident and was pronounced brain dead at the hospital.

Mr. Dunlap told The Epoch Times that he regained consciousness in the hospital after he was pronounced brain dead and his friends and family were saying their goodbyes.
He tried to scream and move, but nothing happened. Since he was an organ donor, he was soon scheduled for organ procurement.
The family prayed for Mr. Dunlap in the hospital. Mr. Dunlap’s cousin, who is a nurse, didn’t believe it was his time.

The cousin conducted additional tests on him. When the cousin pressed under Mr. Dunlap’s thumbnail, Mr. Dunlap pulled his arm to the other side of the body. This movement revoked the diagnosis.
After a few more days, Mr. Dunlap began breathing on his own. He was discharged a month later.
Dr. Varelas, who reviewed media reports on Mr. Dunlap, told The Epoch Times that Mr. Dunlap’s outcomes looked so good that he suspects some steps may have been missed during the assessment.
If doctors had adequate experience with brain-death assessments and diligently followed the AAN’s guidelines, false positives would not occur, said Dr. Varelas.
While his hospital makes 50 to 60 brain-death assessments every year, smaller community hospitals may make very few. Therefore, doctors at these hospitals may not have enough experience, miss signs, or carry out the brain-death assessments out of order, he added.
Dr. Bernat said that the test often performed incorrectly is the apnea test.
Deceptive Death Conditions
The authors of the 2023 AAN guidelines advise that prior to brain-death assessment, all of the following conditions should be eliminated, including:- Hypothermia (low body temperature)
- Autoimmune nervous system diseases
- Drug overdoses
- Poisoning
Autoimmune conditions like Guillain-Barré syndrome, which damages a person’s nervous system, can also rob someone of their reflexes and consciousness.
The patient was admitted to the hospital after showing severe symptoms. Within several days, he became unconscious and unresponsive, lost his brainstem reflexes, and needed a ventilator to breathe.
An apnea test was not conducted. Had the patient been tested in such a way, he would have failed because he would have been too weak to breathe, said Dr. Kim-Tenser.
The patient was then transferred to Dr. Kim-Tenser’s hospital, where he was prescribed autoimmune disease medication. Later, he regained consciousness and some function of his limbs.
Drug overdoses from opioids and cocaine can also cause signs of brain death. An overdose on the muscle relaxant baclofen, for instance, has been known to mimic brain death.
Conflicts of Interest
“There is an intense interest in [brain death] by [organ-procurement organizations], the transplantation community, and patients on organ-waiting lists,” Dr. Varelas wrote in a 2016 article on brain death.Around 90 percent of all organ donors are brain-dead people. This is because the brain-death definition allows surgeons to procure healthy organs without invoking the “dead-donor rule.”
According to the dead-donor rule, an ethical norm, organ donors must be declared dead before organ procurement, and organ procurement must not cause the donor’s death.
Organs cannot be transplanted from people who are biologically dead, which occurs after a person’s heart stops and he or she cannot be resuscitated.
“When you’re biologically dead, the loss of oxygen to your vital organs causes them to decompose so quickly that you cannot donate an organ,” said Dr. Klessig.

That said, tissues like cornea, cartilage, bone, and skin can come from dead donors. Live-organ donation can also be done to transplant the lobe of a lung, liver, or kidney.
Doctors who make brain-death assessments must not be involved in the organ procurement process.
“We try to disassociate ourselves from the organ-donation process,” Dr. Varelas said. “In my mind, we try to save the patient’s life, and that’s the goal because the Hippocratic Oath is to do no harm.”
Nevertheless, conflicts of interest exist. Forty-nine percent of the authors of the AAN’s 2023 guidelines on brain-death assessment reported conflicts of interest related to organ procurement.
Synonymizing brain death with death is an issue of non-transparency, Mr. Miller said. However, he said he would not consider organ procurement unethical as long as the donor is well informed.
In the United States, many people sign up to become organ donors when they apply for a driver’s license, and most of them assume that their organs will only be removed in the case of their death, Dr. Klessig said.
“They think, ‘If I’m as good as done, might as well take my organs anyway,’” Dr. Byrne said.
Still a Mystery
The concept of brain death started half a century ago, a few years after the first organ transplant was successfully performed.Organ procurement from comatose people started in the late 1950s. However, this was rare and not practiced under any guidelines. During the same era came a shift in the definition of death.
On Dec. 3, 1967, the world was astounded by the first report of a successful human heart transplantation performed by Dr. Christiaan Barnard in Cape Town, South Africa. The heart was procured from a trauma victim with massive head injuries. The donor had no brain activity detected on EEG scans and lacked brainstem reflexes. However, her heart continued to beat with life support.
The heart recipient survived for 18 days before succumbing to pneumonia, but his heart functioned properly until his death. This success initiated the practice of heart transplantation.
The chief resident assisting him asked, “Do you think this is really legal?”
“I guess we'll see,” Dr. Shumway said.
They defined irreversible coma as a “new criterion for death,” which has become a foundational cornerstone to the brain-death definition.
Despite this, scientists are still uncertain whether the definition or the consequent assessment is perfect.
Regarding Mr. Dunlap’s recovery, Dr. Varelas said, “I am glad this young man survived.” He believes the family’s prayers for Mr. Dunlap could have contributed to his outcome.
“There are powers much higher than our medical knowledge—or the lack thereof,” he said.
“The secret of life—including the definition of life—still remains the deepest and most mysterious one,” said Dr. Dworkins.
Nature may never “permit anyone to know the exact point where brain death becomes real death,” he added.