What Are the Symptoms and Early Signs of Celiac Disease?
- Diarrhea or constipation
- Abdominal pain
- Bloating and gas
- Heartburn
- Steatorrhea (pale-colored or smelly, fatty stool)
- Nausea or vomiting
- Weight loss
- Nutrient deficiencies (e.g., calcium, copper, zinc, vitamins B6 and D)
- Low blood protein levels
- Electrolyte imbalance
- Fatigue
- Anemia (e.g., iron, ferritin, folate, vitamin B12 deficiencies)
- Headaches
- Itchy, blistering skin rash
- Reproductive changes: male or female infertility, absence of menstrual periods (amenorrhea), miscarriage, premature birth, early menopause
- Recurrent canker sores
- Reduced bone mineral density (osteopenia or osteoporosis)
- Peripheral neuropathy
- Anxiety and depression
- Cognitive impairment
- Impaired spleen function (hyposplenism)
- Elevated liver enzymes
- Failure to thrive
- Growth problems
- Short stature (below the shortest 3 percent for age)
- Swollen belly
- Delayed puberty
- Dental enamel defects
- Irritability
- Attention-deficit/hyperactivity disorder (ADHD) or learning disabilities
- Seizures
What Causes Celiac Disease?

Changes in Bread-Making, Wheat, and Agriculture
Our ancestors, who hunted and gathered food, ate little grain. However, with the development of agriculture, people began eating more grain, especially wheat. Today, wheat is often used as a cheap filler in processed foods, significantly increasing the average person’s gluten intake.In the past, breads, such as sourdough, were fermented. Fermenting can help break down the gluten, making it easier for your body to digest. Today, faster bread-making methods use baker’s yeast or chemicals, which do not help break down the gluten. This shift in bread-making practices, coupled with increased wheat consumption, correlates with the rising rates of celiac disease.
The selective breeding of wheat to enhance yield and resist pests may have made modern wheat strains more immunogenic (immune-provoking) than ancient strains, but not all researchers agree. For those with celiac disease, all strains are problematic.
Genetics
Most people with celiac disease have specific genetic markers called human leukocyte antigen (HLA) types DQ2 or DQ8, with HLA-DQ2 being more common. While up to 40 percent of individuals of European and Asian descent carry these markers, only a few of them develop celiac disease. This indicates that having the genetic markers alone is not enough to cause the disease; other factors, including environmental, also play a role.Environmental Factors
- Processed food: Microbial transglutaminase (mTG) is a food additive used to improve the texture and properties of protein-based foods. This enzyme modifies gluten proteins, making them harder to digest and more likely to trigger an immune response. mTG is similar to tissue transglutaminase, the main target of the immune system in celiac disease. mTG can also disrupt the gut barrier and increase intestinal permeability, making gluten more likely to provoke an immune reaction and contribute to the development of celiac disease.
- Viruses: Certain viruses are also suspected to play a role in the development of celiac disease, especially when inflammation is present. Enteroviruses, rotaviruses, reoviruses, and influenza have been identified as potential triggers. These viruses might influence the gut microbiome, but research is ongoing to understand the mechanisms involved fully.
- Impaired gut microbiome: The gut microbiome—the trillions of bacteria and other microbes in our intestines—plays a crucial role in our immune system and overall health. Increasing evidence suggests that the microbiome may play a major role in the development of celiac disease. In fact, research on germ-free mice shows that gut microbes are required for celiac disease development. Studies have shown that people with celiac disease often have lower levels of beneficial bacteria like Bifidobacteria and Lactobacilli and higher levels of potentially harmful bacteria than those without the condition.
What Are the Types of Celiac Disease?
- Asymptomatic (formerly silent): No noticeable symptoms are present. This type may include at-risk individuals, such as family members of those with celiac disease who are diagnosed through screening. It may also include people with minor symptoms like fatigue not previously linked to celiac disease. If symptoms improve on a GFD, the condition should be reclassified as subclinical. Interestingly, symptoms may become noticeable only after starting a GFD when a previously unnoticed symptom resolves.
- Symptomatic (formerly overt): Either gastrointestinal symptoms or extraintestinal manifestations may be present.
- Classical (formerly typical): Diarrhea, steatorrhea, and weight loss or growth failure are required features of this type. Other signs and symptoms of malabsorption may also be present. Some researchers would prefer this type to be called “intestinal” for clarity. In a few cases, autoantibodies may not be elevated, but villous atrophy (flattened villi) is present. About 27 percent of people fall into this category.
- Non-classical (formerly atypical): Constipation and abdominal pain may be present but without the typical signs of malabsorption. Some researchers prefer to call this type “extraintestinal.” Over half of those with celiac disease have this type.
- Sub-clinical: Signs and symptoms are subtle, not easily detected, or insufficient to prompt testing. About 21 percent of people with celiac disease fall into this category.
- Potential: Autoantibodies are elevated, and inflammation with increased intraepithelial lymphocytes is present, but the intestinal lining appears normal.
- Refractory celiac disease: Symptoms may not resolve after 12 months on a GFD for various reasons that require further investigation. When signs, symptoms, and villous atrophy persist, one potential cause may be refractory celiac disease, a more severe form.
Who Is at Risk of Celiac Disease?
- Age: Celiac disease can develop at any age, but around 25 percent of all celiac disease diagnoses are now made in patients over 60 years old, and 20 percent are among those 65 and older. Some research indicates it’s more common in children than adults, though other evidence suggests it’s more commonly diagnosed in adults, likely due to delayed diagnoses.
- Sex: As with most other autoimmune conditions, females are more likely to develop celiac disease. One 2018 meta-analysis in Clinical Gastroenterology and Hepatology showed that females were 1.5 times more likely to have biopsy-confirmed celiac disease.
- Ethnicity: Celiac disease is more prevalent in individuals of European descent but can affect any ethnicity.
- Geographic region: Celiac disease is most common in Europe and Asia, with significant rates also in North America and Africa. In the United States, the disease is less common in the southern states than in the northern states. This may be due to where studies have been conducted, genetic predisposition, and environmental factors like sunlight exposure affecting vitamin D levels. Evidence shows that vitamin D is vital for immunomodulation in celiac disease and other autoimmune diseases.
- Family history: If you have a first-degree relative (parent, sibling, or child) with celiac disease, your risk of developing it is 5.5 percent to 22.5 percent based on biopsy-diagnosed criteria. Having a second-degree relative (aunt, uncle, grandparent) poses a lower risk, but higher than the general population. Regular screening for family members can help with early detection and treatment.
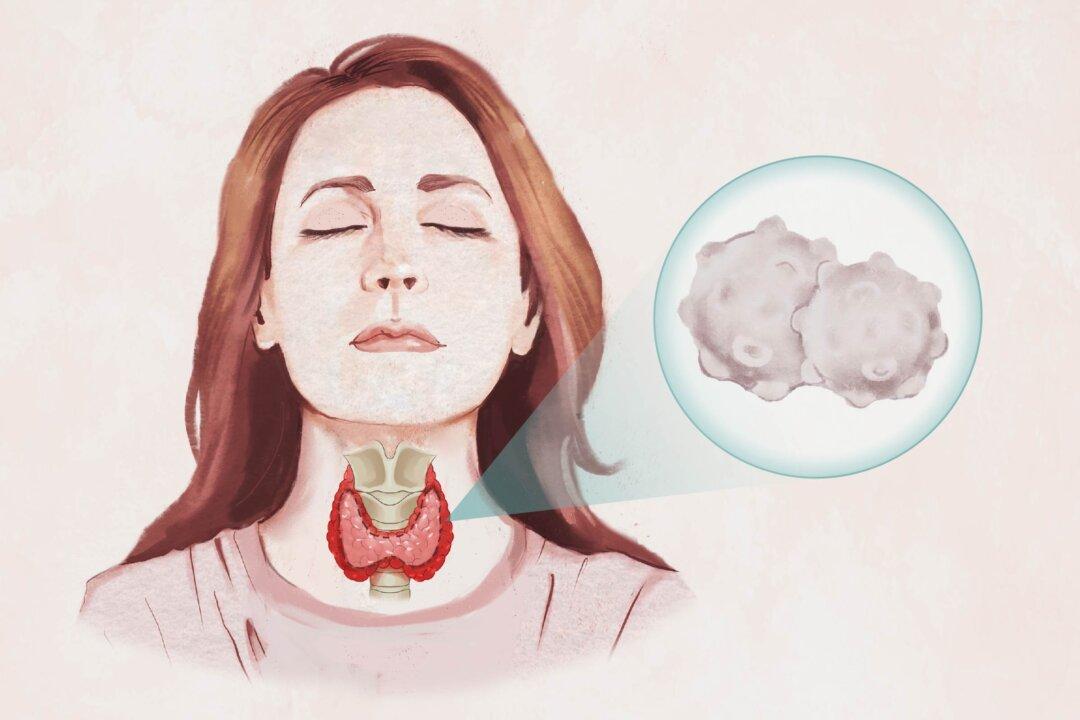
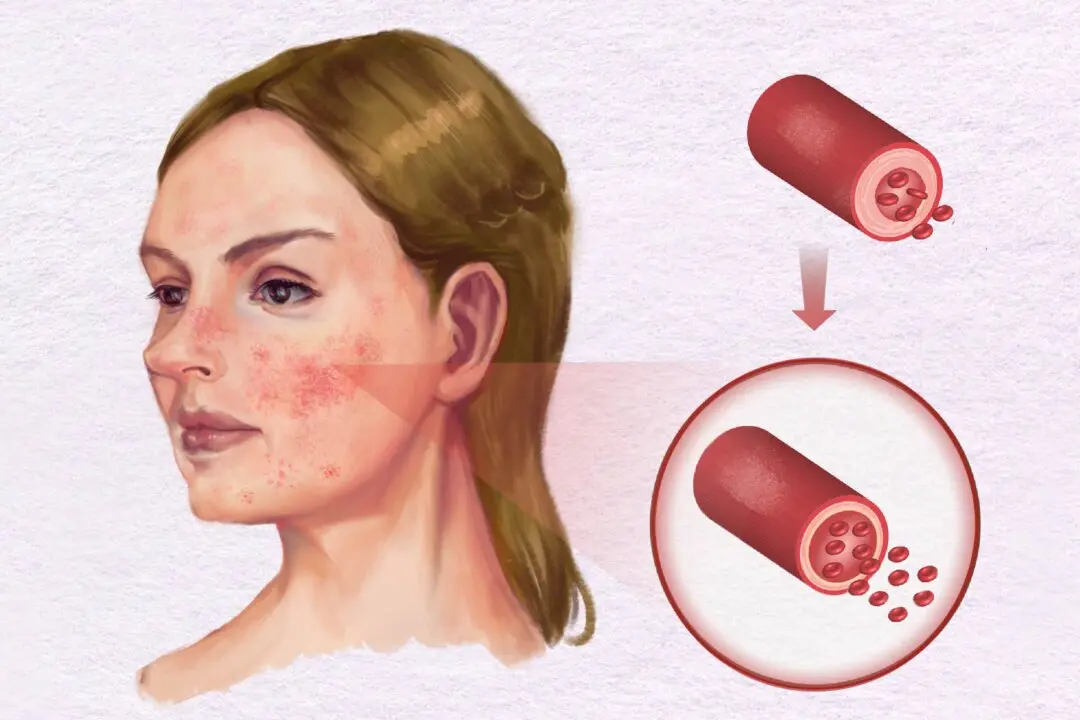
- Autoimmune conditions: Certain autoimmune conditions have up to 10 times the increased risk of celiac disease. These include Type 1 diabetes, Hashimoto’s thyroiditis, Graves’ disease, Addison’s disease, rheumatoid arthritis, Sjogren’s syndrome, multiple sclerosis, autoimmune hepatitis, alopecia areata (hair loss), lupus, and psoriasis.
- Genetic disorders: A high prevalence of celiac disease exists in cases of Down’s syndrome, Turner syndrome, and Williams syndrome sufficient to warrant screening.
How Is Celiac Disease Diagnosed?
Diagnosing celiac disease is complex because no single test is 100 percent accurate or specific, and the results can also vary between laboratories. Therefore, doctors use a multistep process that combines several tests. They look at symptoms, perform blood tests (serology), and review intestinal biopsy results taken during an endoscopy to make a diagnosis.
- Blood tests: Total immunoglobulin A (IgA) levels must be checked because IgA deficiency can produce false positives. Tests look for tTG IgA autoantibodies produced in reaction to gluten. If those are elevated, another test can look for endomysial antibodies IgA in adults and deamidated gliadin peptide IgG in children. If IgA results show a deficiency, tTG IgG and deamidated gliadin peptide IgG tests are recommended. Additional testing can be helpful when skin rash or neurological symptoms are present. While tTG2 is more widely distributed in the body, tTG3 is expressed primarily in the skin, and tTG6 is abundant in the brain and in nerve cells. Antibodies to tTG3 or 6 may be elevated when antibodies to tTG2 are not.
- Genetic tests: While testing for HLA-DQ2 and HLA-DQ8, the genetic markers associated with celiac disease, is not required, guidelines indicate that not having these markers can rule out the disease. However, a Brazilian study showed that 6.8 percent of people with confirmed celiac disease did not have either marker. Thus, ruling out celiac disease solely based on these genetic tests could result in some missed diagnoses.
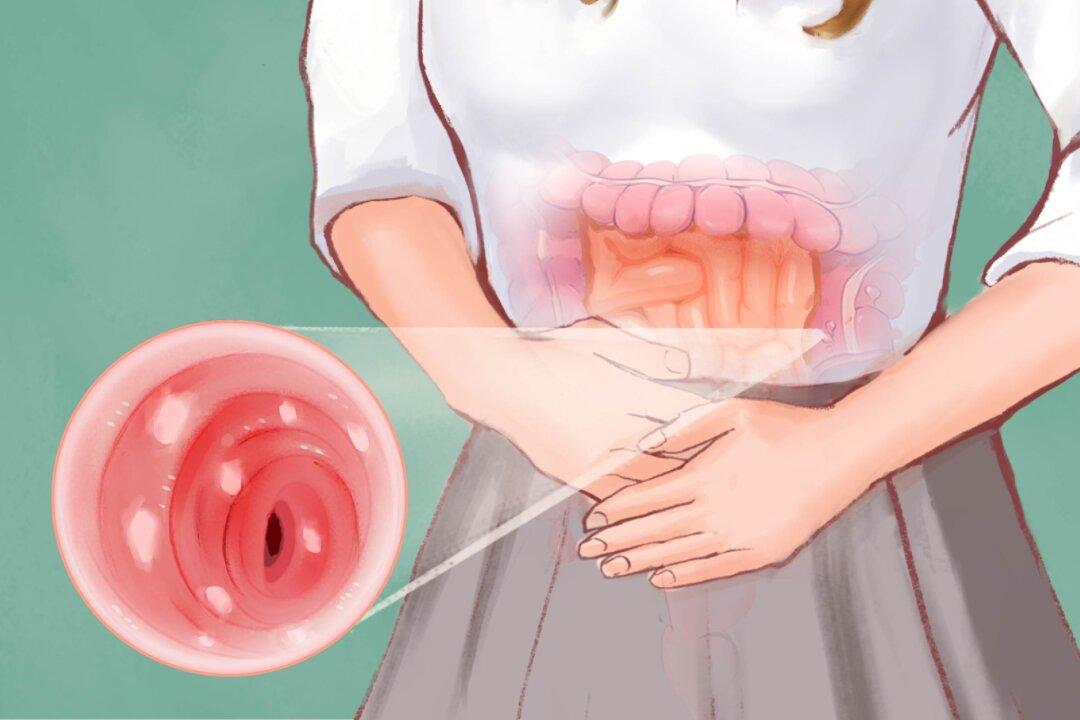
- Intestinal biopsy: Current guidelines recommend confirming the diagnosis with an intestinal biopsy obtained during an endoscopy. The samples are examined for villous atrophy and intestinal damage indicative of celiac disease. Multiple samples (at least four from the distal duodenum and one or two from the duodenal bulb) are recommended because intestinal damage can be unevenly distributed.
- Non-biopsy diagnosis: In select cases where certain criteria are met, a non-biopsy approach may be used for children or adults unable or unwilling to undergo endoscopy. This would include cases where tTG levels are greater than 10 times the upper limit, the person is positive for endomysial antibodies, and the person is positive for HLA-DQ2/DQ8 genetics.
Test Before Going Gluten-Free
Deciding whether to get tested or start a GFD without a confirmed diagnosis is a personal choice. However, getting a formal diagnosis before going gluten-free has many benefits. It helps with medical management, provides social acknowledgment, and can offer financial advantages. Here are some things to consider:- Accurate testing: Although celiac disease symptoms may take a long time to develop initially, once gluten is eliminated, the symptoms with reintroduction can be immediate and more severe. Thus, you may not be able to eat enough gluten for long enough to get accurate test results later, and if you do, significant damage may occur. Furthermore, not all doctors may be willing to do an “after-the-fact” diagnosis, and you may or may not have the genetics required.
- Family screening and support: Confirmation emphasizes the need for family members to be tested to potentially catch the disease early in relatives. It can also strengthen your commitment to a strict GFD and garner support from family and friends.
- Educational and workplace benefits: A formal diagnosis can help you get necessary accommodations in public schools through a 504 plan and in workplaces.
- Insurance coverage and ongoing health care: A diagnosis ensures insurance coverage for treatments and monitoring for nutritional deficiencies, related conditions, and complications.
What Are Possible Complications of Celiac Disease?
- Anemia
- Stunted growth in children
- Osteoporosis and increased fracture risk
- Potential liver disease
- Severe weight loss and muscle wasting (cachexia and sarcopenia)
- Electrolyte imbalance requiring hospitalization
- Lactose intolerance resulting from villous atrophy
- A leaky gut, which promotes ongoing inflammation and an elevated risk of developing intolerances to other foods and autoimmune disorders
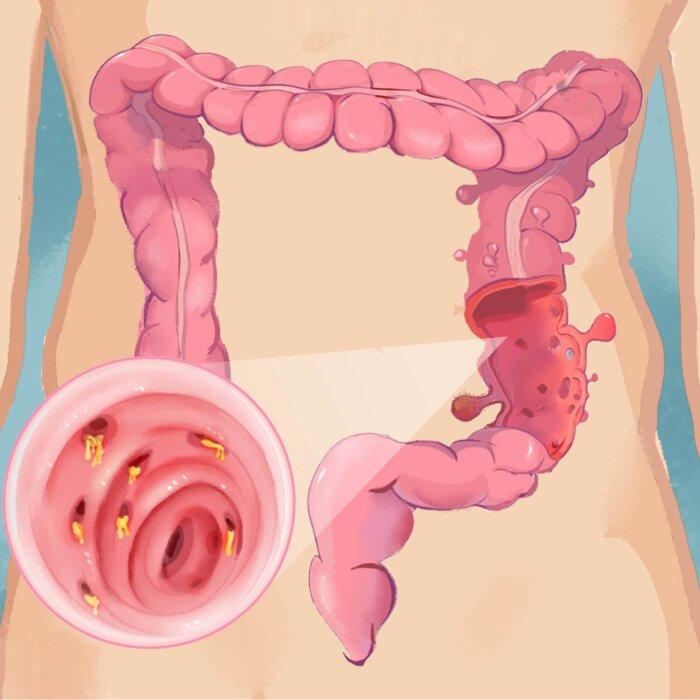
- Intestinal ulcers, scarring, and strictures as observed in ulcerative jejunoileitis (ulcers and scarring in the small bowel)
- Peripheral neuropathy.
- Ataxia (impaired coordination).
- Seizures.
- Potentially increased risk of dementia and Alzheimer’s disease in older people. Prompt treatment may prevent permanent neurological damage and neurodegeneration.
- Anxiety and depression: In one study, 62.7 percent of celiac patients had anxiety, and 34.9 percent had depression.
- Schizophrenia: Some research indicates celiac patients may be at an increased risk of schizophrenia. There is also some debate about a link between the disease and mood disorders, such as bipolar disorder, but the findings have been inconclusive.
- Infertility
- Miscarriage
- Premature births
- A child’s increased risk of developing psychotic disorders later in life for those whose mothers had elevated gluten antibodies to gluten during pregnancy, ranging from 70 percent to 150 percent depending on the antibody levels
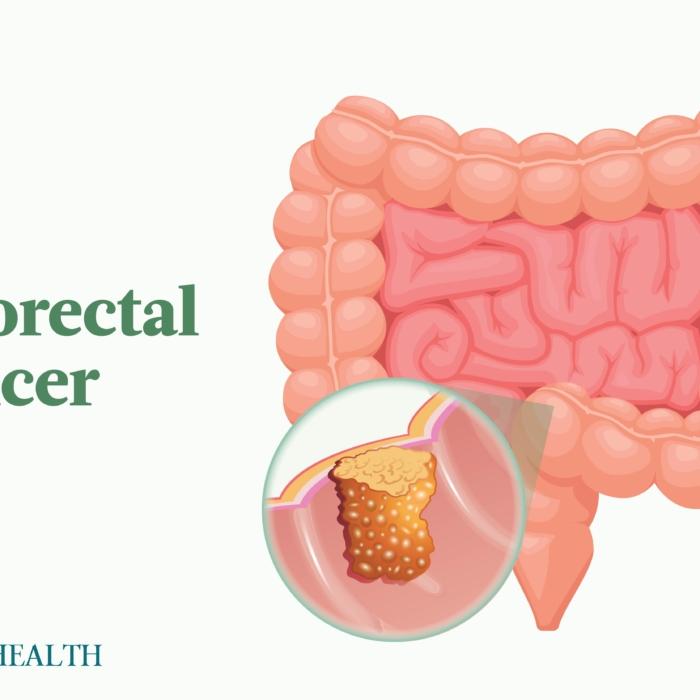
- Small intestinal adenocarcinoma
- Lymphomas like enteropathy-associated T-cell lymphoma (EATL)
- Increased risk of ischemic heart disease, heart attacks, and atrial fibrillation likely due to systemic inflammation
- Increased risk, especially for glomerulonephritis and IgA nephropathy
What Are the Treatments for Celiac Disease?
Health Risks and Nutritional Concerns
It is essential to be cautious when replacing regular foods with gluten-free alternatives. Many processed gluten-free products are higher in calories, fats, sugars, and simple carbohydrates and lower in fiber. Relying too heavily on these options can lead to weight gain, nutritional imbalances, and worsening inflammation, which can potentially contribute to depression and brain fog.Managing Symptoms and Seeking Support
Even with strict adherence to the GFD, healing is a gradual process. While some symptoms will start to abate in weeks, it may take months for gastrointestinal symptoms to resolve fully, a year for bone density to improve, and years for complete healing of the intestinal villi and microvilli. Incomplete healing, characterized by persistent villous atrophy, is relatively common and is most frequently attributed to unintentional gluten exposure.How Does Mindset Affect Celiac Disease?
Adopting an Abundance Mindset
Practicing self-compassion and focusing on the abundance of nutritious foods you can still enjoy can be empowering. Many staple foods, such as fruits, vegetables, nuts, seeds, meats, poultry, and fish, are naturally gluten-free. Additionally, the availability of gluten-free products made from whole grains or higher fiber alternatives like almonds, cassava, chickpeas, and lentil flours has improved dramatically. This progress may make it easier to maintain a balanced diet.Holistic Health Approach
Embracing a nutrient-dense, anti-inflammatory diet based on whole foods not only helps manage the disease but also supports overall physical and mental well-being. A positive mindset can even influence serotonin levels, potentially reducing the risk of depression and anxiety, which are common in untreated celiac disease.What Are the Natural Approaches to Celiac Disease?
A Functional Medicine Approach
A more comprehensive approach may be beneficial to address cross-reactivity and support overall healing. The “5 R’s“ of functional medicine provide a natural approach and framework for reducing overall inflammation, restoring gut barrier function, modulating the immune system, and identifying and eliminating cross-reactive triggers. They are:- Remove: Identify and eliminate factors other than gluten that cause an immune reaction and potentially contribute to inflammation and gut dysbiosis. These include infections, cross-reactive foods, stressors, and toxins. Antimicrobials may be used to treat underlying infections. A food sensitivity test, reactivity test, or elimination diet can help identify problematic foods.
- Replace: Replenish deficient nutrients, enzymes, and acids essential for proper digestion and absorption, enhancing the gut’s ability to heal. Some enzyme supplements may help minimize the effects of accidental gluten exposure, though they will not completely prevent a reaction.
- Reinoculate: Reduce inflammation and support the healing process and a healthy gut microbiome with specific probiotics and prebiotics tailored to your microbial profile, which can be identified through detailed stool testing.
- Repair: Address factors contributing to intestinal permeability, such as stress, alcohol, processed foods, hormonal imbalances, and nonsteroidal anti-inflammatory drugs (NSAIDs). Nutrients like glutamine, zinc, vitamin D, and fiber can support gut healing and barrier function.
- Rebalance: Optimize overall health through balanced nutrition, stress management, regular exercise, and other supportive lifestyle habits to reduce systemic inflammation and promote long-term well-being.
Ayurvedic Herbs
Incorporating Ayurvedic herbs into a natural approach to celiac disease may offer complementary benefits by reducing inflammation and promoting gut healing. A recent study highlighted the potential therapeutic effects of the following herbs:- Turmeric (Curcuma longa): a common spice in Indian cuisine containing curcumin, known for its anti-inflammatory and antioxidant effects
- Ashwagandha (Withania somnifera): an adaptogenic herb with potential anti-inflammatory and gut-healing properties
- Long pepper (Piper longum): a relative of black pepper believed to have anti-inflammatory and immune-modifying properties
- Heart-leaved moonseed (Tinospora cordifolia): an Ayurvedic herb proposed to have anti-inflammatory and immune-modifying properties
How Can I Prevent Celiac Disease?
Deciding to avoid gluten is a personal choice. It is essential to weigh the potential benefits of preventing disease and intestinal damage against the challenges of maintaining a strict GFD.