What Are the Types of Glaucoma?
Primary
- Primary open-angle: Open-angle glaucoma is the most common type in the United States, comprising 90 percent of all glaucoma cases. It is characterized by damage to the optic nerve, a wide anterior chamber angle (the space between the cornea and the iris surface), and increased intraocular pressure (IOP; eye pressure) of over 21 millimeters of mercury (mmHg). This type of glaucoma is a significant cause of blindness, particularly among African Americans, where it accounts for nearly 20 percent of all cases.
- Normal-tension: Normal-tension glaucoma is a form of open-angle glaucoma that occurs in people with regular eye pressure (below 21 mmHg). In the United States, between one-third and one-half of people with glaucoma have this type.
- Angle-closure: Also called narrow-angle or acute glaucoma, angle-closure glaucoma is a medical emergency. It accounts for approximately 10 percent of all glaucoma cases in the United States. The “angle” is where the iris and cornea meet at the outer edge of the anterior chamber. Angle-closure glaucoma occurs when the outer edge of the iris obstructs fluid drainage from the front of the eye, leading to rapid fluid buildup and a sudden rise in pressure. Without prompt treatment, this type of glaucoma can result in severe vision loss or blindness within a few days. Chronic angle-closure glaucoma progresses gradually and may not exhibit symptoms other than vision loss.
- Primary congenital: Primary congenital glaucoma is a rare condition resulting from improper development of the aqueous drainage system before birth. It affects approximately 0.01 percent of babies born in the United States.
Secondary
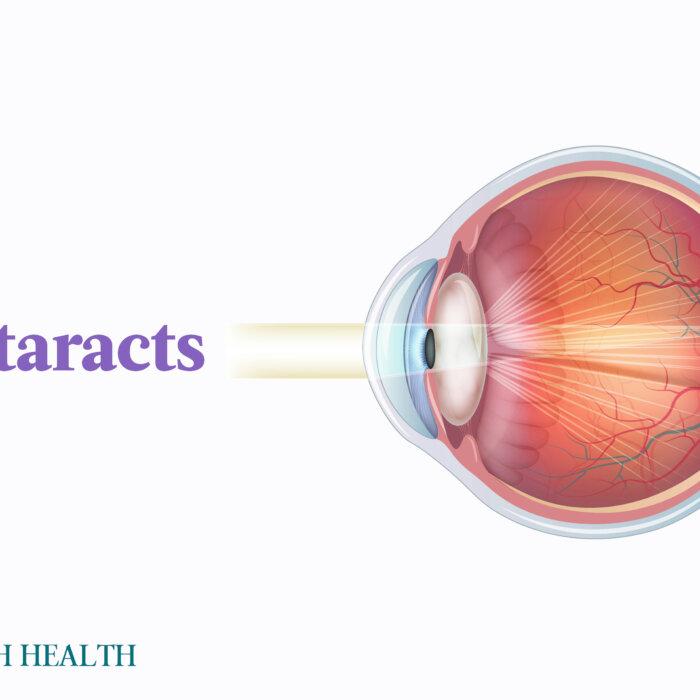
Other medical conditions, such as cataracts, tumors, diabetes, eye surgery complications, and the use of certain medications can also cause the following glaucomas:- Neovascular: Neovascular glaucoma occurs when excessive blood vessel growth obstructs the eye’s drainage area, typically due to underlying medical conditions such as diabetes or high blood pressure.
- Pigmentary: Pigment dispersion syndrome occurs when pigment rubs off from the back of the iris, potentially increasing eye pressure and causing pigmentary glaucoma.
- Exfoliation: Exfoliation glaucoma, also known as pseudoexfoliation glaucoma, is a form of secondary open-angle glaucoma occurring in individuals with exfoliation syndrome. This syndrome leads to the accumulation of cellular material on various parts of the eye, thus obstructing fluid drainage.
- Uveitic: Uveitic glaucoma is a common complication of uveitis, which causes eye swelling and inflammation. Around 20 percent of people with uveitis develop uveitic glaucoma. Experts believe inflammation and scar tissue formation in the eye’s middle region may block fluid drainage, leading to increased eye pressure, uveitic glaucoma, and eventual vision loss.
- Secondary childhood: Secondary childhood glaucoma results from an eye developmental anomaly unrelated to the aqueous drainage system, a syndrome, or another eye condition.
What Are the Symptoms and Early Signs of Glaucoma?
- Primary open-angle: This type is nicknamed “the silent thief of sight” as patients often experience no symptoms until vision damage becomes significant when blind spots start developing in the side vision. The symptoms include increased IOP and tunnel vision.
- Normal-tension: Patients typically don’t experience symptoms until it’s too late, which is the same for people with open-angle glaucoma (except open-angle exhibits elevated IOP). Patients may also experience bleeding in the nerve fiber layer of the optic disc.
- Angle-closure: Symptoms include severe eye pain, nausea, red eye, and blurred vision. If you suddenly experience these symptoms, seek medical attention immediately.
- Primary congenital: Children diagnosed with congenital glaucoma often exhibit cloudiness in their eyes, light sensitivity, abnormally high tear production, and possibly larger-than-normal eye size.
- Neovascular: Symptoms include eye pain or redness and loss of vision.
- Pigmentary: Individuals with pigment dispersion syndrome or pigmentary glaucoma may experience halos (rainbow-colored rings around lights) or blurred vision following activities such as jogging or playing basketball.
- Exfoliation: While exfoliation glaucoma shares the same symptoms as primary open-angle, it can advance more rapidly and frequently results in increased eye pressure.
- Uveitic: Uveitic glaucoma can damage the optic nerve and induce a loss of visual field. Patients with it experience symptoms of both uveitis and glaucoma, including red eyes, pain, sensitivity to light, spots in vision, and blurred vision.
What Causes Glaucoma?
Usually, this fluid moves like water filling a sink. The faucet (the ciliary body) produces it, and drains (drainage canals) remove it from the eye to maintain a normal fluid level. As drainage canals become clogged, the fluid doesn’t drain properly, resulting in an imbalance. When pressure becomes abnormally high, it harms the optic nerve, leading to glaucoma.
Low- or normal-tension glaucoma can occur when eye pressure is within the normal range but still too high for the optic nerve.

- Age: African Americans 40 years old and above and people of all ethnicities who are 60 years old and above (particularly Hispanics) are at a higher risk of developing glaucoma. Males in their 30s are at the highest risk for pigmentary glaucoma, with the ratio of males to females ranging from 2:1 to 5:1, depending on the study.
- Ethnicity: African Americans have a significantly higher risk of developing glaucoma—about six to eight times—than whites. Normal-tension glaucoma seems to affect those of Japanese ancestry more. Higher risks for angle-closure glaucoma are seen in Asian and Inuit populations, with lower risks in European and African populations.
- High intraocular pressure: Intraocular pressure (IOP) is the leading risk factor for glaucoma.
- Family history of glaucoma: Researchers have identified specific genes that may affect people’s risk of glaucoma. Identical twins with the same genes are more likely to have glaucoma than fraternal twins, hinting that genetics play a role.
- Eye structure: Thin corneas, thinning of the optic nerve, concave iris, posterior iris insertion, and flat corneas are risk factors for pigmentary glaucoma.
- Cardiovascular issues, like heart conditions and abnormal blood pressure.
- Eye-related conditions, such as reduced optic nerve tissue, retinal detachment, eye tumors, and eye inflammation, can make one more prone to glaucoma. Retinal ischemia and systemic vascular conditions put one at risk of neovascular glaucoma.
- Farsightedness or nearsightedness.
- Eye injury.
- High blood pressure increases your risk of open-angle glaucoma.
- Diabetes is a risk factor for open-angle glaucoma.
- Low blood pressure can make one more likely to develop normal-tension glaucoma.
- Low birth weight can increase the risk of primary congenital glaucoma.
- Maternal history of seizure increases one’s risk of inheriting primary congenital glaucoma.
- Medications: In addition to people with uveitis, people taking steroids, which can treat uveitis, can develop uveitic glaucoma. Also, a new study found a link between attention-deficit/hyperactivity disorder (ADHD) medications and angle-closure and open-angle glaucomas.
- Lifestyle: Some lifestyle activities that can raise IOP include playing high-wind instruments, drinking coffee, practicing specific yoga poses, wearing tight neckties, and lifting heavy weights. One 2022 study found a link between snoring, daytime sleepiness, insomnia, and both short and long sleep durations and the risk of developing glaucoma. Stress is also a factor, as chronic stress can affect various organs, and the eyes are no exception. Glaucoma patients often link severe emotional stress to their vision problems; this connection is supported by research showing that stress can increase eye pressure and cause vascular issues in the eye and brain, potentially leading to reduced oxygen and glucose levels (which can hurt eye health). While nerve cells may not die outright, they may become inactive and negatively affect vision.
- Heavy metal toxicity: The connection between glaucoma and certain neurodegenerative disorders suggests that heavy metal (e.g., cobalt, lead, mercury) toxicity could contribute to glaucoma development.
- Ionizing radiation: Ionizing radiation can potentially contribute to the development of glaucoma, particularly in cases of high doses of prolonged exposure.
How Is Glaucoma Diagnosed?
- Tonometry: Tonometry uses a tonometer to measure the pressure inside the eye. During the test, your doctor applies a small amount of anesthetic and dye to the eye’s front, then shines a light into the eye and gently touches its surface with the tonometer. Some optometrists use a puff-of-air instrument that doesn’t touch the eye. Normal eye pressure ranges from 11 to 21 mmHg, with readings above 21 mmHg considered high. Serial tonometry involves taking multiple pressure measurements over a period of time and observing how eye pressure changes throughout the day.
- Optic nerve evaluation: To check for changes in the optic nerve, your doctor uses an ophthalmoscope, which consists of a light source and magnifying lenses, to see inside the eye. Sometimes, other tools are used, such as optical coherence tomography, a scan that uses special light rays to create an image of the back of your eye. This optic nerve assessment can show if glaucoma has caused any damage.
- Visual field testing: A visual field test, also known as perimetry or a peripheral vision test, assesses for any areas of vision loss. During the test, you’ll see a series of light spots, with some appearing at the edges of your vision, to test your peripheral vision, which is typically affected first by glaucoma. If you can’t see these spots in your peripheral vision, it could indicate vision damage from glaucoma.
- Gonioscopy: Gonioscopy uses a special lens to inspect the eye’s drainage canals to determine whether the glaucoma is open-angle or closed-angle.
- Corneal thickness measurement: Your doctors will also assess corneal thickness, as thinner corneas may increase the risk of glaucoma. Corneal thickness can also affect the accuracy of eye pressure readings. Thinner corneas might lead to underestimated readings, while thicker corneas may lead to higher readings.
- Visual acuity test: A visual acuity test, often using an eye chart, assesses your ability to see clearly at different distances.
- Eye muscle function test: An eye muscle function test assesses the muscles around your eyes for any issues. During the test, your doctor will move an object and ask you to track it with your eyes.
- Slit-lamp exam: The slit-lamp examination assesses the front structures of the eye using a specialized microscope with a bright light. It helps doctors evaluate various eye parts, such as the eyelids, cornea, conjunctiva, sclera, and iris, in detail.
What Are the Complications of Glaucoma?
- Blindness: This is usually painless.
- Painful blind eye: Having open-angle glaucoma increases the risk of a condition called central retinal venous occlusion, which may lead to a painful blind eye.
- Visual field loss.
- No light-perception vision: No light perception refers to the most severe type of vision loss, with a complete inability to detect light. This condition usually indicates an advanced or end-stage disease, as all sensory input from the eye is lost.
What Are the Treatments for Glaucoma?
Currently, there is no cure to reverse vision loss caused by glaucoma. However, treatment can help prevent additional damage and further vision loss based on the type and severity of the condition. In some cases, eye drops may not effectively control eye pressure. Your doctor might recommend an oral medication—often a carbonic anhydrase inhibitor—to help lower eye pressure.
1. Eye Drops
Eye drops are commonly used as an early treatment for glaucoma; it’s crucial to use them regularly to manage eye pressure effectively. Usually, eye drops are initially applied to one eye (known as a one-eye trial). If there’s improvement in the treated eye within one to four weeks, then both eyes will receive treatment.Before using an eye drop, inform your doctor about any other medications or supplements you are taking, as the eye drops may interact with these substances.
- Prostaglandins: Examples are latanoprost, travoprost, tafluprost, and bimatoprost. Possible side effects may include slight eye irritation, changes in eye color, and elongated eyelashes.
- Rho kinase inhibitors: Rho kinase inhibitors improve fluid drainage in the eye through a pathway called the trabecular meshwork. Examples include netarsudil and ripasudil. Possible side effects include redness and discomfort in the eye.
- Nitric oxides: Nitric oxides help lower IOP by decreasing the production of aqueous humor, making it easier for fluid to flow out through a central drainage canal, and relaxing the trabecular meshwork cells. These functions improve the drainage of fluid from the eye. Examples include latanoprostene bunod and NCX 470.
- Miotic or cholinergic agents: Due to side effects such as head and eye pain and potential vision changes, as well as the need for their frequent use of up to four times daily, this type of medication is not commonly used anymore. One example is pilocarpine.
- Alpha-adrenergic agonists: Typically, these medications are administered two or three times daily. Their possible side effects include irregular heart rate, increased blood pressure, red or itchy eyes, dry mouth, and fatigue. Examples are apraclonidine and brimonidine, with brimonidine being the anti-glaucoma alpha agonist of choice.
- Beta blockers: Potential side effects include decreased heart rate, reduced blood pressure, breathing difficulties, and fatigue. Examples include betaxolol and timolol.
- Carbonic anhydrase inhibitors: These medications are usually taken two or three times daily. Possible side effects may include a metallic taste, increased frequency of urination, and tingling sensations in the fingers and toes. Examples include dorzolamide and brinzolamide.
2. Laser Treatment
When both eye drops and oral medications don’t suffice, laser treatment may be recommended, as it’s effective for certain types of glaucoma. It involves using a focused beam of high-energy light on your eye to reduce or prevent fluid buildup and lower the eye pressure. Different types of laser treatments include the following:- Laser trabeculoplasty involves using a laser to widen the drainage tubes in your eye, thus improving fluid drainage and lowering internal pressure.
- Cyclodiode laser treatment uses a laser to remove eye tissue that produces fluid to reduce eye pressure.
- Laser iridotomy is designed for individuals with angle-closure glaucoma. During this procedure, an ophthalmologist uses a laser to make a small hole in the iris to facilitate fluid flow to the drainage angle in the eye.
3. Surgery
Many types of glaucoma surgery are available, including:- Trabeculectomy: This is the most common type of surgery used for glaucoma treatment. During the procedure, a surgeon makes a small flap in the sclera (the white part of the eye) to create a drainage path for fluid. This type of surgery, typically considered when other treatments have failed, may have complications such as vision loss, cataracts, infection, and droopy eyelids. Patients are often awake during this surgery, as only a local anesthetic is used, although general anesthetic is also available.
- Trabeculotomy: Trabeculotomy is very similar to trabeculectomy, except it uses an electric current to cut the sclera.
- Viscocanalostomy: Viscocanalostomy involves removing a portion of the sclera to facilitate easier fluid drainage from the eye.
- Glaucoma implant surgery: A surgeon inserts a small tube (shunt) onto the eye’s sclera during this procedure. This shunt helps drain excess fluid.
- Minimally invasive glaucoma surgery (MIGS): MIGS is a newer approach for mild glaucoma with fewer risks and side effects than conventional surgeries. It reduces eye pressure to aid faster recovery. While showing promise for certain glaucoma types, MIGS is currently not considered universally superior to other treatments.
- Deep sclerectomy: Deep sclerectomy widens the drainage channels in your eye, often achieved by inserting a small device into them.
- Cataract surgery: Cataract surgery can often lower eye pressure in people with cataracts, making it a potential treatment for glaucoma in some cases.
4. Novel Treatment Methods in Development
Researchers are developing several new treatment approaches for glaucoma, such as cell-based therapies for optic nerve regeneration. While promising, these approaches are in the early research stages and not yet ready for human clinical trials.How Does Mindset Affect Glaucoma?
Maintaining a positive mindset can reduce mental stress, a potential cause of glaucoma. It can also help lower eye pressure, a key factor in glaucoma management, and reduce vascular dysfunction.
What Are the Natural Approaches to Glaucoma?
1. Medicinal Herbs
According to a 2002 survey of 1,000 glaucoma patients, 5.4 percent used alternative treatments for their glaucoma, and 57.4 percent of those used herbal therapies. Some popular herbs for this condition include:- Ginkgo (Ginkgo biloba): A 2013 retrospective study assessed 42 patients with treated normal-tension glaucoma who were given 80 milligrams of ginkgo biloba extract twice daily. The extract slowed the progression of visual field damage in these patients. In a 2003 study, 27 patients with vision loss due to normal-tension glaucoma were given either ginkgo biloba extract or a placebo. The extract was taken orally, three times daily for four weeks, followed by an eight-week washout period, then four weeks of placebo. The researchers conducted visual field tests at different stages and discovered that the extract might help improve existing vision loss in some patients.
- Bilberry (Vaccinium myrtillus): Bilberry contains anthocyanin, a flavonoid that may protect nerve cells and help with glaucoma. It could improve blood flow to nerve cells, strengthen the optic nerve, make nerve cells more resistant to damage, and reduce eye inflammation. In one 2017 study, the retinal ganglion cells of mice given bilberry extract orally were protected from dying. The extract increased certain proteins related to cell protection, which may explain its ability to protect against eye injuries such as those in glaucoma. Another 2012 retrospective study involving 332 glaucoma patients found ginkgo and bilberry extracts beneficial for enhancing vision in certain people with normal-tension glaucoma.
- Chinese skullcap (Scutellaria baicalensis): Chinese skullcap extract and its main active flavonoids, including baicalin, baicalein, and wogonin, have low toxicity and can protect nerves, fight oxidative stress, reduce inflammation, and even combat cancer. These flavonoids can protect against damage caused by reduced blood flow in the retina. One 2015 study discovered that baicalein treatment in animals lowered eye pressure by enhancing fluid drainage from the eye. Another 2016 study found that administering wogonin in a rat model with optic nerve crush decreased the loss of their retinal ganglion cells and prevented these cells’ apoptosis.
- Saffron (Crocus sativus): Crocin, crocetin, and safranal are the key components behind saffron’s beneficial health effects. These compounds can protect against DNA damage, act as antioxidants, fight cancer, reduce inflammation, prevent heart disease, control blood sugar and pressure levels, improve lipid profiles, and delay degenerative conditions. One 2019 study discovered that a type of saffron extract reduced inflammation and protected cells in the eye, particularly the retinal ganglion cells, in mice with high eye pressure.
- Erigeron breviscapus: Erigeron breviscapus is a flowering plant native to China that belongs to the Asteraceae family. A 2011 study showed that treating rabbits with chronic increased IOP with an Erigeron breviscapus extract for 60 days protected retinal nerve cells. Scutellarin, extracted from Erigeron breviscapus, possesses cardioprotective properties against conditions such as ischemia, heart attack, stroke, and diabetic complications. A 2021 study on mice with chronic IOP elevation found that oral scutellarin helped maintain the mice’s retinal structure and vision, suggesting that scutellarin could be a new treatment option for glaucoma.
- Qing Guang An Granule (QGAG): A 2020 study examined QGAG, a Chinese medicine used to treat glaucoma for over two decades, and identified 55 active compounds and 173 targets related to glaucoma treatment. Among them, 20 key targets were found to be involved in processes such as cell death, response to oxygen deficiency, and cell growth regulation. The researchers also discovered critical pathways suggesting that QGAG may offer the potential for further research and new drug development for glaucoma treatment.
2. Supplements
- Vitamin C: Vitamin C, known to exist in high concentrations in the human eye, is believed to interact with oxygen in eye fluids. Since it can reduce oxidative damage in cells, vitamin C can potentially protect against retinal damage in glaucoma. A 1966 study found that intravenous glycerol-vitamin C (sodium salt) could lower pressure inside the eye. However, newer studies are needed to confirm vitamin C’s IOP-reducing function.
- Alpha-lipoic acid (ALA): Alpha-lipoic acid is an antioxidant derived from caprylic acid, a medium-chain fatty acid found in foods like coconut. It’s produced in the mitochondria and plays a role in breaking down nutrients. There’s ALA in red meat, beets, carrots, potatoes, spinach, and broccoli. In one 2013 study, researchers gave ALA to mice with glaucoma symptoms to see if it could stop the disease from deteriorating and to another group of mice before they developed glaucoma to see if it could prevent the disease. The results showed that both approaches increased eye cell protection, improved cell transport, and reduced oxidative stress, which is linked to glaucoma.
- Melatonin: Melatonin is a hormone that our brains produce in the dark. Supplements can be used to treat jet lag, anxiety, and certain sleeping disorders. A 2006 review suggested that certain retinal ganglion cells play a role in the release of melatonin. Considering this connection, using drugs that affect melatonin could be a promising addition to the treatment of glaucoma, along with traditional methods that focus on managing eye pressure.
3. Other
The following are other natural approaches that may help with glaucoma symptoms:- Acupuncture: One 2020 systematic review found that acupuncture might slightly reduce eye pressure. Another 2018 study showed that acupuncture targeting specific acupoints around the eyes can enhance blood flow in people with primary open-angle glaucoma. However, further research with better-designed trials is still needed.
- Changing sleeping position: The head-up position at 20 degrees is associated with lower nighttime eye pressure than lying flat (supine).
- Exercise: Engaging in treadmill exercise and regular physical activity can lead to a temporary decrease in IOP.
- Achieving ideal BMI: A 2020 study found that Korean women with low BMI had higher rates of glaucoma, possibly due to lower nutrient intake. Another study found that individuals with a BMI over 30 were more likely to develop primary open-angle glaucoma. Additionally, metabolically healthy obese people were at a lower risk than metabolically unhealthy non-obese people. Metabolic health is affected by things like diabetes, hypertension, and high cholesterol.
- Relaxation techniques: Meditation and other relaxation techniques may help lower stress and help optimize glaucoma treatment.
How Can I Prevent Glaucoma?
- Eat more fruits and vegetables: One 2012 study found that consuming more fruits and vegetables (e.g., oranges, collard greens, and spinach) rich in vitamins A and C, along with carotenoids, might lower the risk of glaucoma in older African American women. A 2016 study linked the consumption of dietary nitrate and green leafy vegetables to a reduced risk of primary open-angle glaucoma.
- Stay physically active.
- Avoid head-down positions: Spending too much time upside down, like when using gravity tables, increases eye pressure, which raises glaucoma risk.
- Proactively manage stress.
- Stay current with annual comprehensive dilated eye exams: If you are in a high-risk group or over 40, getting a complete yearly exam is recommended.
- Don’t smoke.
- Maintain oral health: Some research suggests a link between gum disease and glaucoma.
- Wear protective eyewear when needed to avoid eye injury.
- Treat underlying medical conditions that may lead to glaucoma.
- Reevaluate the need for certain medications, like steroids, which raise your risk of glaucoma with prolonged use.