Rosacea, a chronic inflammatory condition, affects at least 16 million people in the United States and more than 5 percent of the global population. Its visible signs on the face, such as redness, flushing, dilated blood vessels, bumps, and thickened skin, can profoundly impact self-esteem and social life for those affected. Notable individuals with rosacea include former President Bill Clinton, Karl Malden, Cameron Diaz, and Renee Zellweger.
Emerging research suggests rosacea is more than just skin-deep. It is a systemic disorder with complex causes, including genetics, dysfunctional immunity, and environmental factors. This makes managing rosacea difficult, often requiring ongoing treatment and lifestyle adjustments to control symptoms. The recurring nature of rosacea flare-ups can lead to scarring and permanent skin thickening, adding to the difficulties faced by those dealing with the condition.
What Are the Types of Rosacea?
Rosacea manifests in several distinct forms or subtypes. Individuals may experience symptoms of more than one subtype at the same time or progress from one type to another. The four primary subtypes of rosacea are as follows:
- Erythematotelangiectatic rosacea (ETR): This is the most common type, represented in over 50 percent of cases with redness, flushing, and dilated blood vessels visible on the face.
- Papulopustular rosacea (PPR): This is also known as “acne rosacea.”
- Ocular rosacea: This type affects the eyes and eyelids and can sometimes be the first sign of rosacea, appearing before any other skin symptoms.
- Phymatous rosacea: This rare form is caused by an overgrowth of sebaceous glands and connective tissue. It most commonly affects the nose but can also involve the chin, forehead, cheeks, and ears.
What Are the Symptoms and Early Signs of Rosacea?
The signs and symptoms of rosacea can vary significantly depending on the subtype, each marked by distinct clinical features. While rosacea most commonly appears on the forehead, cheeks, nose, and chin, it can also appear on other parts of the body, but these cases are not well-documented. Dilated blood vessels, which appear as fine red or purple lines that may look like a web or a branching pattern, are sometimes called spider veins.
Here are the key features of each rosacea subtype.
Erythematotelangiectatic Rosacea (ETR)
- Flare-ups with symptoms coming and going
- Central facial flushing and redness (erythemato)
- Visible spider veins (telangiectasia)
- Swollen, sensitive skin
- Burning or stinging sensation
Papulopustular Rosacea (PPR)
- Breakouts persisting for weeks or months
- Red, swollen bumps (papules)
- Pus-filled bumps (pustules)
- Sensitive skin
- Visible spider veins
Phymatous Rosacea
- Thickening (phyma) and bumpy skin texture, often appearing as a bulbous nose (rhinophyma)
- Enlarged pores
- Visible spider veins
Ocular Rosacea
- Watery, bloodshot eyes
- Burning or stinging sensation in the eyes
- Dry, itchy eyes
- Light sensitivity
- The sensation of something in the eye
- Inflamed bumps resembling styes
- Crusty buildup along the eyelid margins
- Irregular eyelid edges
- Diminished vision
- Visible spider veins on the eyelids
What Causes Rosacea?
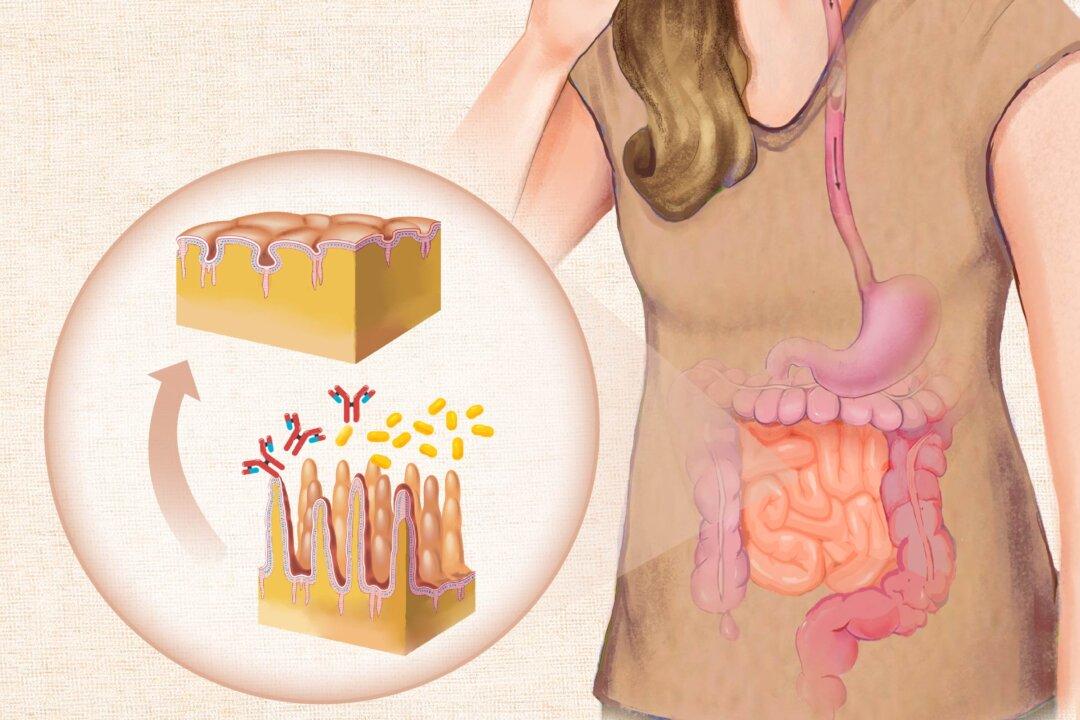
In rosacea, inflammation compromises the skin’s natural barrier, leading to alterations in the skin’s microbiome. These changes further exacerbate inflammation, perpetuating a vicious cycle that can be challenging to interrupt. Effectively managing rosacea and its varied symptoms requires strategies that disrupt this cycle, addressing both the symptoms and their underlying causes.
Rosacea’s causes are complex and not fully understood. Rosacea involves complex, self-perpetuating cycles driven by a combination of genetic, environmental, and biological factors. Key elements that have been identified in the development include:
- Genetic predisposition: Several genetic variations have been linked to the development of rosacea. However, having these genetic factors alone does not necessarily mean a person will get rosacea. Environmental and lifestyle factors can influence genetic expression, playing a pivotal role in whether rosacea symptoms develop.
- Environmental triggers: The top 10 triggers that can start or worsen symptoms include sun exposure, stress, hot weather, wind, heavy exercise, alcohol consumption, hot baths, cold weather, spicy foods, and humidity.
- Immune system dysregulation: Rosacea is associated with abnormalities in both the innate and adaptive immune systems, leading to an overactive immune response and chronic inflammation, a central feature of the condition.
- Vascular and neurovascular dysfunction: Disturbed interactions involving blood vessels and nerves contribute to the characteristic redness and flushing, which then feed back into the inflammatory cycle.
- Impaired skin barrier: The skin barrier is the outermost layer that protects the body from external threats. In rosacea, the skin loses the normal balance in hydration and also loses the tight junctions between the skin cells. As a result, the skin becomes more sensitive and reactive to irritants, which can worsen inflammation.
- Microbial dysbiosis: Imbalances in the natural bacteria and microbes on the skin and gut are associated with rosacea. This includes an overgrowth of certain microbes, such as Demodex mites on the face, Bacillus oleronius, Staphylococcus epidermidis, and potentially Helicobacter pylori (H. pylori). These microbial imbalances can exacerbate the immune response and inflammation.
- Metabolic disturbances: Conditions such as insulin resistance and abnormal cholesterol levels may share common pathways with rosacea, influencing its progression.
- Oxidative stress response: High stress levels within the cells, such as oxidative stress, can interfere with normal cell function and contribute to rosacea development.
- Abnormalities in the skin’s oil-producing glands: Rosacea involves changes in the type and makeup of the oils that the skin’s sebaceous glands produce. These alterations in the skin’s natural oils can play a role in both the onset and exacerbation of rosacea symptoms.

Although its exact cause is unknown, rosacea typically results from some combination of genetic predisposition, environmental factors, and biological disturbances, such as microbial or microbiota imbalance, oxidative stress, or an overactive immune system. (Illustrations by The Epoch Times, Getty Images)
In some cases, symptoms similar to rosacea may arise from sources other than the condition’s primary causes. For instance, prolonged use of topical corticosteroids can lead to steroid-induced rosacea. Amiodarone, a medication for treating heart rhythm disorders, has also been linked to these symptoms. Similarly, calcineurin inhibitors like tacrolimus and pimecrolimus, often used to treat rosacea, can paradoxically worsen or trigger them.
Moreover, rosacea-like symptoms can manifest due to underlying systemic diseases, such as gastrointestinal or autoimmune disorders. In such instances, working with a health care professional to identify and address the root causes is essential.
Who Is at Risk of Rosacea?
Certain factors can make someone more likely to develop rosacea, including:
- Age: Rosacea can occur at any age but more commonly occurs after age 30, which is also when severity peaks. The prevalence decreases in older people, likely due to changes in the immune system or skin physiology.
- Sex: Some studies indicate rosacea occurs more in women than men, while others show no difference. However, it tends to happen earlier in women, and in men, rhinophyma is more common, as is the likelihood of the condition progressing to advanced stages.
- Ethnicity: Rosacea is most commonly reported in fair-skinned individuals, particularly those of Northern European descent. While rosacea can affect people of all skin colors, it might be underdiagnosed in those with darker skin because symptoms are less visibly apparent.
- Family history: Up to 30 percent of those with rosacea have a family history of the condition. Additionally, a twin study indicates genetics may account for 50 percent of the risk for developing rosacea.
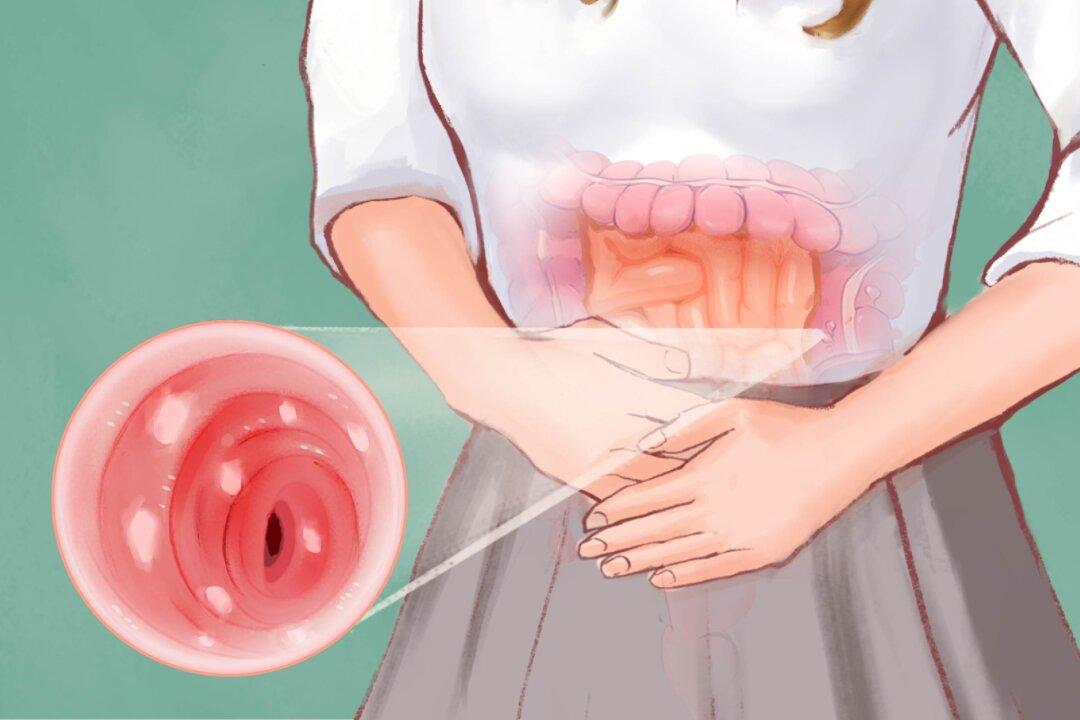
- Inflammatory bowel disease (IBD): There seems to be a bidirectional association between rosacea and IBD, with rosacea being more common in people who have either form of IBD—Crohn’s disease or ulcerative colitis—and vice versa.
- Lifestyle: Obesity and smoking are significant risk factors for developing rosacea.
How Is Rosacea Diagnosed?
Rosacea is diagnosed through a physical skin examination and a detailed review of the patient’s medical history and symptoms. Tests or biopsies may be performed to exclude other conditions like psoriasis, eczema, lupus, or sarcoidosis. However, there is no specific laboratory test for rosacea.
Diagnostic Criteria
The following features are considered diagnostic for rosacea, with only one required:- Persistent facial redness: This core feature involves ongoing facial skin redness (generally over three months) that may worsen periodically due to certain triggers.
- Phymatous changes: This involves thickening or enlargement of the skin, often noticeable on the nose.
Major Features
The major features below are not diagnostic alone, but the presence of two or more can be considered diagnostic if none of the above diagnostic criteria is present:- Flushing (transient redness of the facial skin)
- Inflammatory papules and pustules on the face
- Spider veins on the facial skin
- Ocular manifestations, including red and inflamed eyelids, itchiness (blepharitis), and inflammation affecting various parts of the eye—cornea, conjunctiva, and sclera—that can cause discomfort, redness, and potential vision issues.
Minor Features
Health care practitioners may also note the presence of minor features such as a burning or stinging sensation, dry skin, and swelling (edema). While these are not required for diagnosis, they can support the overall assessment.In addition, the diagnosis of ocular rosacea requires either of the following:
- Both visible dilated blood vessels along the eyelid margins and redness or inflammation of the white part of the eye
- Abnormalities or irregularities of the cornea (the clear front part of the eye) and inflammation of the white part of the eye
Functional Medicine Testing
Beyond the conventional diagnostic approach, functional or integrative practitioners may order tests to identify potential underlying factors or triggers. This might include the following:- SIBO (small intestinal bacterial overgrowth) breath test to detect problems with the gut microbiota
- Stool test to assess gut dysbiosis, inflammation, and infections like H. pylori
- Blood tests to assess autoimmunity, metabolic health markers like methylation and oxidative stress, nutrient levels, or fatty acid balance
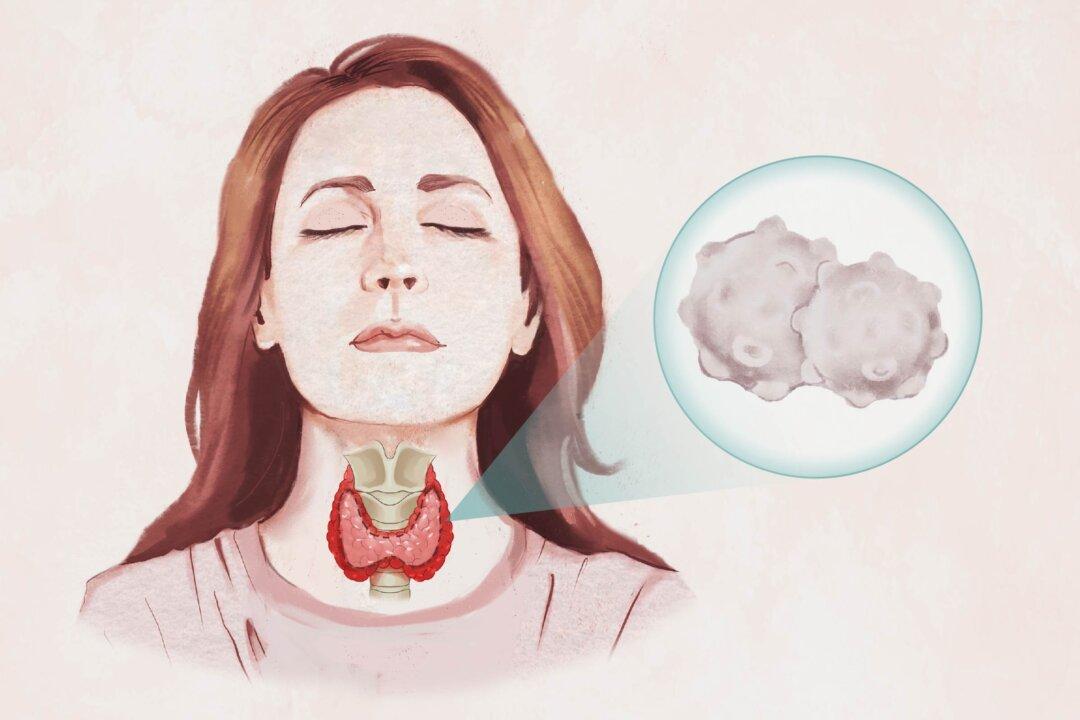
- Hormonal tests to identify any imbalances in sex hormones, thyroid function, or adrenal hormones that could be contributing to or exacerbating rosacea symptoms
What Are the Complications of Rosacea?
While rosacea is not life-threatening, it can be progressive. If left untreated, it can lead to various complications and consequences, including:
- Permanent skin changes: Persistent redness, flushing, and inflammation from rosacea can result in permanent changes such as scarring, deformation, and thickening of the skin on the nose, which may require surgery if obstructing the nasal passages (otherwise, it is considered cosmetic).
- Eye complications: Potential consequences of ocular rosacea include rosacea keratitis, an inflammation of the cornea, corneal scarring, and surface irregularities, all of which may impair vision.
- Increased cancer risk: Research suggests a link between rosacea and an increased risk of certain cancers, including nonmelanoma skin cancer and breast cancer. A weaker association was found with glioma, a type of brain cancer, indicating a higher risk in men than in women. There appears to be no link between rosacea and melanoma, and the evidence is conflicted for associations with other cancers, like those of the thyroid and liver.
- Dysbiosis: While imbalances in the gut microbiome may aggravate rosacea symptoms, the reverse could also be true given the bidirectional gut-skin axis. Additionally, systemic antibiotic treatment of rosacea could disrupt the microbial balance.
- Morbihan disease: This is a rare complication characterized by chronic, progressive facial swelling and redness, often affecting the upper two-thirds of the face. This condition can lead to significant facial disfigurement and visual impairment.
- Increased risk of other conditions: Some research has associated rosacea with an increased risk of certain other medical conditions, such as IBD, cardiovascular disease, dementia, anxiety, and depression. However, the causal nature of these relationships has not been established.
- Psychosocial impact: Visible signs of rosacea often lead to embarrassment, low self-esteem, social anxiety or phobia, and frustration. Additionally, lifestyle may be limited in an attempt to avoid triggers. These psychosocial effects can significantly impair mental health and quality of life.
What Are the Treatments for Rosacea?
Treating rosacea requires a tailored approach to manage its various symptoms and subtypes. Conventional treatments focus on addressing the specific features of rosacea, with the choice of therapy guided by the severity and subtype. Be sure to discuss potential adverse events and antibiotic resistance with your prescribing health care providers.
Topical therapies targeting the particular rosacea symptoms are often the first-line approach for mild to moderate cases. These can help reduce facial redness, inflammation, papules, and pustules. In more severe or treatment-resistant situations, oral systemic medications, laser- or light-based treatments, or surgical options may be considered. Combination therapy can also be an effective approach, with a combination of topicals commonly used for maintenance.
The treatment options outlined in the table below provide a comprehensive overview of the targeted therapies health care professionals use for the different rosacea subtypes.
How Does Mindset Affect Rosacea?
Your mindset and rosacea have a two-way relationship, so it is essential to consider both. Rosacea and its treatments can really affect how you feel mentally and emotionally. People with rosacea are more likely to experience anxiety, depression, and a lower quality of life compared to others, often struggling socially.
Feeling self-conscious about your looks, dealing with lifestyle limitations, unexpected flare-ups, constant medical treatment, and the costs involved can all add up to a lot of stress. But emerging research suggests that having a positive mindset might not only help you cope with stress better but also could affect how well your treatment works.
One study found that using cognitive behavioral therapy (CBT) techniques could help rosacea patients feel less anxious and depressed while also increasing their sense of control over the condition. CBT has also been shown to lower inflammation, so getting help with your mindset and coping strategies could be invaluable for managing your rosacea. Moreover, people who had rosacea for a shorter time had better quality of life scores, suggesting that early psychological support may enhance treatment response.
Stress can disrupt the delicate balance in your microbiome, promoting inflammation and exacerbating rosacea. By having a more positive outlook and using stress-management techniques, you might be able to ease some of the inflammatory processes that drive your rosacea symptoms. Being actively involved in your treatment and setting achievable goals can also positively affect your sense of control and well-being.
What Are the Natural Approaches to Rosacea?
Conventional medical treatments are essential for managing rosacea symptoms, but combining them with an integrative, natural approach that targets root causes can provide a more comprehensive solution. The following evidence-based natural strategies may reduce rosacea flare-ups and improve long-term skin health and overall well-being.
1. Gut Health Support
Microbial imbalances associated with rosacea can contribute to increased intestinal permeability, or “leaky gut.” This altered barrier may allow toxins and bacteria to enter the bloodstream, where the immune system sees them as foreign invaders. This can trigger an inflammatory immune response and rosacea symptoms. Consider these gut healing strategies:- Treat infections: Treat any underlying conditions like SIBO or H. pylori infections, which may respond to herbal therapies or pharmaceuticals. Certain herbal remedies have shown effectiveness in resolving these gut imbalances.
- Avoid triggers: Identify and eliminate food sensitivities or trigger foods. A detailed symptom journal can help pinpoint foods and other triggers that activate your immune system and create inflammation. Foods that commonly cause immune reactions include gluten, dairy products, fried foods, and artificial additives, though these vary individually.
- Supplement nutrients: If your dietary intake is deficient, incorporate gut-healing nutrients, such as vitamin D, zinc, and L-glutamine, to help repair the intestinal barrier.
- Sip bone broth: Bone broth components, including collagen, amino acids, and chondroitin sulfate, may benefit gut health and reduce inflammation, though direct effects on rosacea are not confirmed.
- Try probiotics: Incorporate probiotic supplements or fermented foods with live probiotics to help restore beneficial gut bacteria and improve microbiome diversity. Consult a qualified health care professional to select the right probiotic strain. Although Lactobacillus acidophilus LA5 and Bifidobacterium lactis Bb12 may help with decreasing H. pylori density, other strains of the Lactobacillus acidophilus and Bifidobacterium lactis species might not have the same effect.
- Incorporate prebiotics: Eat prebiotic-rich foods, like fiber-containing fruits and vegetables and gluten-free whole grains, to nourish the beneficial gut microbes.
- Boost essential fatty acids: Research indicates that omega-3 fatty acids (fish, fish oil, seeds, nuts), specifically eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA), can improve blood flow and may have anti-inflammatory effects, help improve dry eye symptoms, and reduce redness and inflammation in patients with rosacea, particularly in ocular rosacea.
2. Skin Care and Botanicals
Proper skin care is crucial for managing rosacea, focusing on gentleness to minimize irritation and enhance skin health. Here are some key strategies:- Makeup removal: Use a gentle, oil-based product to remove makeup without harsh scrubbing. Gently remove makeup with your hands (instead of cloth, etc.) and use a light touch. Exfoliation is not recommended, as it is too abrasive and will aggravate rosacea.
- Cleansing: Choose a soap-free cleanser for sensitive skin and use lukewarm water to avoid irritation.
- Facial massage: Incorporating a gentle facial massage into your routine may enhance circulation and help reduce swelling.
Light green or yellow-tinted makeup can help temporarily conceal redness, but choosing noncomedogenic, fragrance-free formulas free of harsh chemicals is essential to avoid further irritation.
Alongside these skin care practices, certain plant-based or botanical ingredients in skin care products offer anti-inflammatory and soothing benefits. These effects can be synergistic due to the multiple compounds in botanicals, making them effective for rosacea management. The following are several botanicals and their specific properties that can help alleviate symptoms and improve skin health:
- Colloidal oatmeal: anti-inflammatory, soothing, skin-barrier repair
- Feverfew extract: anti-inflammatory, soothing, blood vessel-sealing
- Licorice root extract: reduces inflammation, improves skin barrier function
- Green tea extract: antioxidant-rich, anti-inflammatory, soothing, blood vessel-sealing
- Coffeeberry: anti-inflammatory, soothing
- Artemisinin (sweet wormwood): anti-inflammatory, restricts the formation of new blood vessels
3. Immune System Support Strategies
Consuming a wide variety of colorful fruits and vegetables can help provide a range of antioxidants and anti-inflammatory compounds to support the immune system. Additionally, staying adequately hydrated can help support the production and circulation of lymph, which carries white blood cells and other immune system cells throughout the body.Zinc supports gut and immune health and has antioxidant and anti-inflammatory properties. Its effectiveness in treating rosacea has varied, with one study showing that 100 milligrams taken three times daily improved symptoms. This dose is still considered high, especially compared to another study, where 220 milligrams was ineffective. High doses of zinc can affect copper levels, so it’s important to balance both minerals. Always consult a health care professional to determine the correct dosage and maintain mineral balance.
4. Cannabis
Early research suggests cannabis and its compounds like CBD may help with rosacea, but more evidence is needed to confirm its effectiveness.How Can I Prevent Rosacea?
Some experts believe rosacea may be preventable by addressing underlying factors other than genetics, while others argue that, since its exact cause is unknown, prevention is impossible. In either case, flare-ups may be prevented and managed. Managing the condition long term requires a multifaceted approach addressing both environmental and lifestyle factors. The following evidence-based strategies may help prevent or minimize rosacea symptoms:
- Environmental factors: Avoid potential triggers such as extreme temperatures, hot baths, humidity, and direct sun exposure. Apply nontoxic sunscreen such as zinc oxide daily, even on cloudy days, and use protective clothing and wide-brimmed hats, and seek shade when outdoors. For those required to wear masks, opt for medical or surgical masks over N95 respirators when possible, take 15-minute breaks every two hours, and use gentle, fragrance-free cleanser every morning and night. Use noncomedogenic moisturizer one hour before wearing.
- Lifestyle factors: Refrain from smoking and consuming alcohol. Aim for at least seven hours of restful sleep per night, engage in regular but moderate exercise, and practice stress reduction techniques such as meditation, yoga, or deep breathing exercises.
- Nutritional deficiencies: Maintain optimal levels of vitamins C and D to support immune function. Vitamin C can also help strengthen blood vessels and reduce oxidative stress.
- Diet: Follow a nutrient-dense, anti-inflammatory diet with organic vegetables and fruit, healthy fats, and meat, fish, and eggs from naturally raised animals. Avoid foods that may trigger flare-ups or are known allergens, and reduce intake of processed foods, sugars, trans fats, and seed oils.
- Microbiome: Support a healthy, balanced gut microbiome through an appropriate diet and probiotic supplementation.