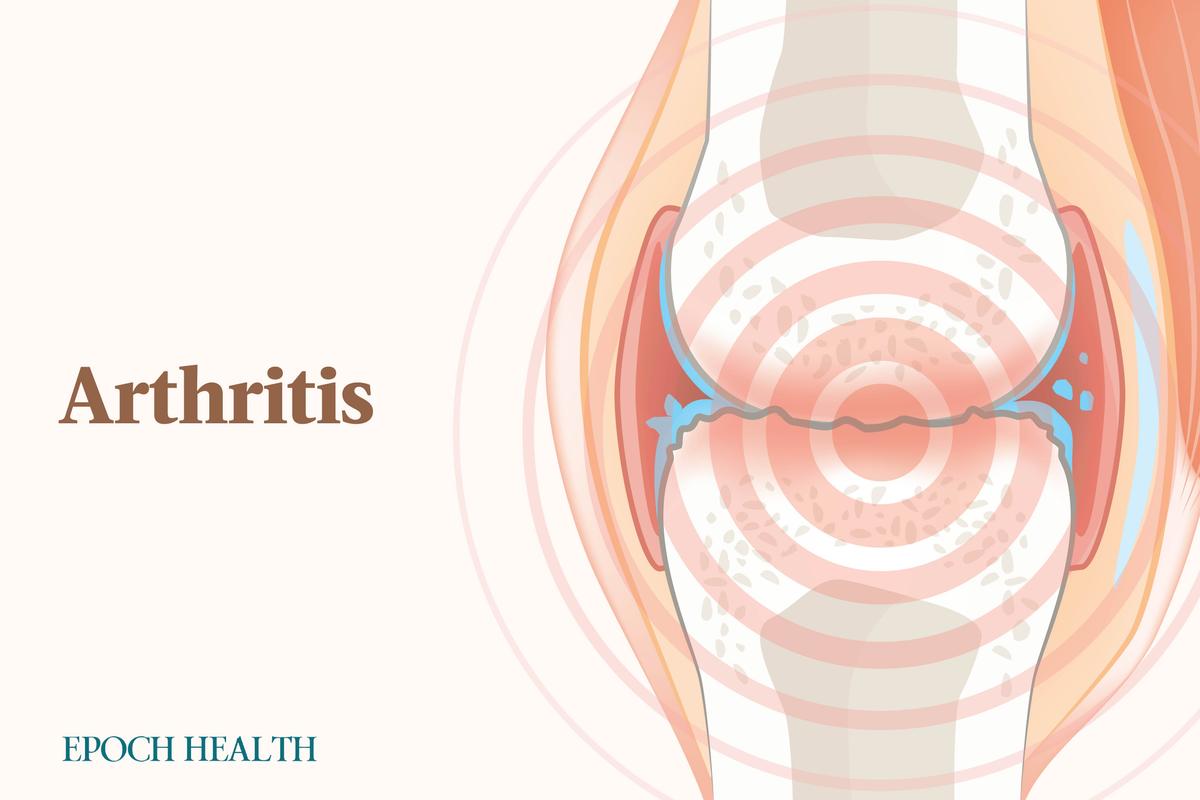
Anatomy of a Joint
Soft tissues cushion your joints and prevent bones from grinding on one another. Articular cartilage, a connective tissue, enables joints to move without pain or friction.What Are the Common Types of Arthritis?
There are over 100 types of arthritic conditions, including the following:Osteoarthritis
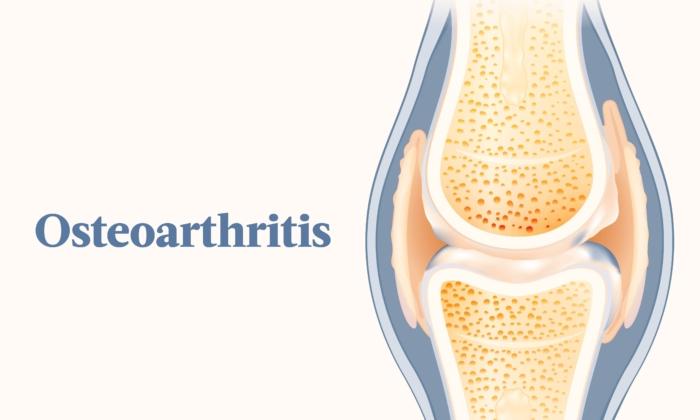
Osteoarthritis is joint degeneration, a form of arthritis that results from stress on the joint that breaks down joint cartilage. It is the most common form of arthritis and typically affects the hands, hips, and knees.Rheumatoid Arthritis
The second most common type of arthritis is rheumatoid arthritis, an autoimmune disease. With rheumatoid arthritis, the immune system attacks the synovial fluid within the joints. This attack on the joints results in joint inflammation, most often in the hands, knees, and ankles. Commonly, it involves the same joint on both sides of the body. In rare cases, rheumatoid arthritis can also cause problems with the eyes, heart, and lungs.Gout
This type of arthritis causes the formation of uric acid crystals in the joints. It affects one joint at a time, causing inflammation and swelling. The most common joint affected is the big toe. This condition gets progressively worse.Ankylosing Spondylitis
Ankylosing spondylitis is also known as arthritis of the spine and usually occurs in the lower back. It may also cause inflammation in the knees, ankles, and hips. This spine arthritis can cause fusion of the vertebrae, leaving the spine rigid and inflexible. People with this type of arthritis may also develop an eye disease called uveitis, psoriasis, or inflammatory bowel disease.Juvenile Arthritis
Also known as juvenile idiopathic arthritis, this type affects children 16 years old or younger by attacking tissue around the joints. The most common form of juvenile arthritis is juvenile idiopathic arthritis, a chronic condition affecting about 300,000 children under 18. Unless they receive aggressive treatment, those diagnosed with juvenile arthritis will have persistant active arthritis 10 years after diagnosis.Psoriatic Arthritis
Psoriatic arthritis develops in people with psoriasis, a condition that causes red and scaly skin, and causes inflammation and pain. On average, up to 30 percent of people with psoriasis will develop psoriatic arthritis. This type is similar to rheumatoid arthritis in its presentation of symptoms but tends to affect fewer joints.What Are the Symptoms and Early Signs of Arthritis?
Some symptoms are shared among all types of arthritis, while some are specific to certain types. Common arthritis symptoms are:- Pain.
- Tenderness.
- Redness.
- Stiffness.
- Warmth.
- Swelling.
- Symptoms lasting at least six weeks.
- Morning stiffness.
- Symptoms affecting more than one joint.
- Fatigue.
- Low-grade fever.
A child having a morning limp may indicate juvenile arthritis. Children can experience flare-ups of symptoms that never go away, or many may never experience the symptoms again after the flare-up.
What Causes Arthritis?
In general, arthritis forms in the following steps:- Joint inflammation (including from overuse, immune response, and uric acid crystals).
- Joint damage.
- Joint stiffening.
- Joint growth is altered (abnormal overgrowth, erosion, etc.).
Osteoarthritis
Osteoarthritis can be caused by wear and tear on the joints. The wear and tear break down the cartilage at the joints, causing pain, discomfort, and decreased range of motion.Rheumatoid Arthritis
An autoimmune condition, rheumatoid arthritis results from the body attacking itself, identifying parts of the joint as foreign to the body. The triggered immune response results in attacks on those parts of the joints.
Gout
The cause of gout is hyperuricemia, a condition involving high uric acid levels in the body. When you eat, purines naturally present in the body and in many foods break down. When there is too much uric acid, uric acid crystals build up in the body’s joints, fluids, and tissues, causing pain and inflammation. Hyperuricemia doesn’t always lead to gout.Ankylosing Spondylitis
The cause of ankylosing spondylitis is unknown, though researchers believe genetics and environment have roles to play. The HLA-B27 gene, in particular, is known to predispose a person to developing this form of arthritis, but having the gene does not guarantee one will develop it.Juvenile Arthritis
The exact cause of arthritis in children is unclear. However, while juvenile arthritis is not hereditary, scientists believe genetics are involved. Still, it is unusual for children in the same family to have juvenile arthritis. It’s possible an environmental factor, such as a virus, can cause this type of arthritis.Psoriatic Arthritis
Researchers don’t know what causes psoriatic arthritis, but it is likely that a combination of genes, environmental factors, and individual immunity contribute to its development.
Who Is at Risk for Arthritis?
Factors that put you more at risk for arthritis are the following:- Participation in sports: Certain sports and physical activities may stress joints repeatedly.
- Autoimmune diseases: The body’s immune system attacks the components of the joints.
- Viral infections: Viruses can cause joint inflammation.
- Age: Arthritis is more common in older people.
- Smoking: Smokers have a higher level of inflammatory proteins.
- Sex: Women are more likely to get arthritis, though men are more likely to develop gout.
- Obesity: A heavier weight can put undue stress on joints.
- Joint injury: Injuries can cause or worsen existing arthritis.
- Race: Some Asian populations have a lower incidence of osteoarthritis.
- Inflammatory bowel disease: Fifteen to 20 percent of Crohn’s disease patients and 10 percent of people with ulcerative colitis will experience arthritis (especially ankylosing spondylitis).
- Human leukocyte antigen (HLA) class 2 genotypes: These genes can make people more susceptible to arthritis or worsen existing conditions
- Family history: Certain types of arthritis can run in families.
How Is Arthritis Diagnosed?
Diagnosis of arthritis begins with a physical exam. During the exam, the health care professional will ask about your symptoms, health history, and how the joint pain has affected your life. He or she will also assess your joints’ range of motion, pain, tenderness, and swelling.Other than the health history and physical exam, your physician may order tests to confirm an arthritis diagnosis or determine the type of arthritis.
- Bone fractures.
- Joint dislocation.
- Cartilage breakdown.
- Muscle injuries.
- Tendon injuries.
- Ligament injuries.
- Soft tissue inflammation.
Blood tests can help diagnose gout by detecting uric acid in the blood. Other tests that identify inflammation can diagnose rheumatoid arthritis. A health care provider can diagnose psoriatic arthritis with a blood test examining erythrocyte sedimentation rate (ESR), determining how quickly red blood cells accumulate at the bottom of a test tube. The faster and heavier they clump together, the more severe the inflammation.
What Are the Complications of Arthritis?
Many complications are associated with arthritis, with several present in only some types of arthritis. Some of the complications of the discussed types are as follows:Rheumatoid Arthritis
Complications of rheumatoid arthritis include:- Eye problems, such as dryness, pain, inflammation, redness, light sensitivity, and sight impairment.
- Dry mouth and gum inflammation or infection.
- Shortness of breath due to lung scarring and inflammation.
- Damaged nerves, skin, and organs due to inflamed blood vessels.
- Low blood cell count.
- Inflamed heart.
- Weight gain due to difficulty exercising regularly.
Ankylosing Spondylitis
Complications of ankylosing spondylitis include:- Pain, stiffness, and swelling in other joints like ribs, shoulders, knees, and feet.
- Shortness of breath if ribs are affected.
- Eye inflammation.
- Fatigue.
- Loss of appetite.
- Weight loss.
- Abdominal pain.
- Loose stools.
- Psoriasis.
Juvenile Arthritis
Juvenile arthritis can negatively impact bone growth and development. Joints may grow unevenly, resulting in one leg or arm being longer or shorter than the other. Children may also develop eye inflammation, which can lead to cataracts, glaucoma, or blindness if untreated.Psoriatic Arthritis
Complications of psoriatic arthritis include those from decreased exercise and inefficient use of iron by the body:- Diabetes.
- High blood pressure.
- High cholesterol.
- Obesity.
- Fatigue.
- Anemia.
What Are the Treatments for Arthritis?
There is no cure for arthritis. Medications and other therapies may minimize the symptoms and complications of arthritis. In the worst cases, a health care professional may recommend surgery.Medications
Medications commonly used to treat arthritis are nonsteroidal anti-inflammatory drugs (NSAID) such as ibuprofen and other anti-inflammatory drugs. Acetaminophen may also help with pain relief. Viscosupplementation is an injection that may be used to lubricate joints.- Colchicine: This drug is used to prevent gout attacks but is not without side effects. Some side effects are less severe, such as nausea and vomiting, while others are more severe, such as unusual bleeding and decreased male fertility.
- Corticosteroids: These are fast-acting anti-inflammatories. Because of the side effects, corticosteroids should not be used long-term but can be used for months. Some side effects include spikes in blood sugar, high blood pressure, and mood changes. Corticosteroids are used for gout, ankylosing spondylitis, and juvenile arthritis. Some corticosteroids include cortisone, prednisone, and methylprednisolone.
- Biologics: These medications are used for rheumatoid, psoriatic, and juvenile arthritis and ankylosing spondylitis. They comprise large molecules produced in living cells that stop or decrease inflammation. Infection is a risk because these medications depress a person’s immune system. Common biologics include adalimumab, rituximab, anakinra, and abatacept.
- Janus kinase (JAK) inhibitors: JAK inhibitors are disease-modifying anti-rheumatic drugs (DMARDs), non-biologics used for ankylosing spondylitis, psoriatic arthritis, and rheumatoid arthritis. These medications are available only as pills. There are three JAK inhibitors: tofacitinib, baricitinib, and upadacitinib. These medications come with the risk of infection.
- Disease-modifying anti-rheumatic drugs (DMARDs): DMARDs are anti-inflammatory drugs used for juvenile arthritis and other types of arthritis. All DMARDs come with the risk of infection. Biologics and JAK inhibitors both fall into this drug class.
- Immunosuppressives: Originally used to prevent organ rejection for transplants, these are now used to treat autoimmune diseases such as psoriatic arthritis and rheumatoid arthritis. Immunospuresants include DMARDs and include the same risks associated with those. Methotrexate can be used to treat severe psoriatic arthritis and stubborn rheumatoid arthritis.
Surgery
For severe cases, surgery may be necessary. Joint repair and replacement are two types of surgical options. If you have severe ankylosing spondylitis, one surgical option is laminectomy, which relieves pressure on nerves. You may also have surgery to straighten the spine or fix fractures. Other surgeries may include the replacement of hip, ankle, shoulder, and knee joints due to arthritic damage.Other Therapies
Besides medications and surgery, other therapies may address the symptoms or complications of arthritis. Such treatments include the following:- Physical therapy: Guided exercises help with muscle and joint function.
- Occupational therapy: These interventions are used to find easier ways to continue with daily activities and promote independence.
- Exercise: Exercise improves mobility and posture to manage pain and slow disease progression.
- Heat or cold applications: Hot or cold compresses can ease joint pain. Heat may lubricate joints, whereas cold reduces inflammation.
- Ultraviolet light treatment: Light treatment, ultraviolet A (UVA), ultraviolet B (UVB), or psoralen plus UVA (PUVA), can reduce inflammation present in psoriatic and rheumatoid arthritis.
- Biofeedback: Biofeedback retrains how your brain experiences pain and stress.
How Does Mindset Affect Arthritis?
Mental health can affect how a person experiences the symptoms and complications of arthritis.People with depression and anxiety are also less likely to follow their treatment plans, which can increase the chances of acquiring other health conditions.
What Are the Natural Approaches to Arthritis?
While there is no cure for arthritis, several natural approaches can help manage it.Supplements
Herbal and dietary supplements have shown promising results in minimizing the symptoms and complications of arthritis. However, data do not sufficiently support most of these claims, and further research is needed.- Glucosamine with chondroitin sulfate: These may decrease knee osteoarthritis pain with minimal side effects. However, do not take glucosamine if you have an allergy to shellfish. Glucosamine may also raise blood sugar, so be aware of this if you have diabetes. Do not take it if you take an anticoagulant or anti-platelet medication, as chondroitin can interfere with these drugs.
- Frankincense (Boswellia serrata): This botanical has anti-inflammatory, analgesic, and anti-arthritic properties. One systematic review and meta-analysis found frankincense extract improved pain, stiffness, and joint function after one month of use. Another study found it increased physical function without serious side effects.
- Curcumin: Curcumin, the bioactive compound in turmeric, has anti-inflammatory and antioxidant effects by inhibiting the production of inflammatory mediators. One study found it to be safer and have fewer adverse effects than the NSAID diclofenac. It was also shown to reduce knee pain with minimal side effects.
- Eremostachys laciniata: A decoction comprising the roots and flowers of this Iranian herb is traditionally given to relieve inflammatory conditions like arthritis. A single-blinded, randomized clinical trial showed that applying a 5 percent ointment of E. laciniata significantly reduced pain scores after two weeks.
- Chamomile: Chamomile is traditionally used to treat joint pain. Compared to other drugs and placebo, chamomile oil significantly decreased the need for acetaminophen and had no adverse events.
- Ginger: Ginger is well known for its ability to reduce inflammation. A study in which participants received two tablets of 500 milligrams of ginger daily for 12 weeks revealed improved pain scores and increased patient satisfaction with no side effects differing from treatment prescribed by orthopedic specialists.
- Calcium: Getting enough calcium is especially important for arthritis patients being treated with corticosteroids.
- Vitamin D: Vitamin D may help to decrease the risk of osteoarthritis and rheumatoid arthritis. People with inadequate vitamin D intake are also likely to have their osteoarthritis worsen three times faster than those with adequate intake.
Nutrition
The food you eat has a huge bearing on your overall health. Eating the right foods can also ease the burden of living with arthritis.Eating a diet rich in whole foods and avoiding processed foods can help with inflammation and joint pain.
- Fish is a good source of omega-3 fatty acids. These may help to decrease inflammation. Fish oil may help reduce swelling in joints and morning stiffness.
- Nuts and seeds are also anti-inflammatory because of their monounsaturated fat content.
- Fruits like strawberries, raspberries, blueberries, and blackberries have anti-inflammatory and antioxidant properties. Vitamin C in fruit helps with inflammation, as does vitamin K. Vitamin K can be found in broccoli, spinach, lettuce, kale, and cabbage.
- Olive oil also contains healthy fats and oleocanthal. Oleocanthal has similar properties to NSAIDs.
- Beans contain anti-inflammatory compounds, phytonutrients, and fiber.
- Whole grains can help you maintain a healthy weight due to their filling fiber content.
- Sugary drinks.
- High-fructose corn syrup.
- Alcohol.
- Game and organ meats.
- Turkey.
- Certain seafood (herring, mussels, scallops, tuna, trout, cod, haddock).
- Yeast.
- Red meat.
How Can I Prevent Arthritis?
You can do some things to lower your chances of developing arthritis or minimize your risks. Modifying the following behaviors can help prevent arthritis:- If you smoke or chew tobacco, quit.
- Avoid high-impact exercises.
- Maintain a healthy body weight.
- Minimize the risk of joint injuries such as fractures and dislocations.
Aerobic exercise that increases your heart rate is also essential. Such activities can improve cardiac health and encourage weight loss, easing joint stress.
- Choosing low-impact exercises such as elliptical trainers and doing exercises in water.
- Applying heat before exercising to relax joints.
- Going slow.
- Icing joints after exercise.