What Are the Common Types of Pancreatic Cancer?
There are two categories of pancreatic cancer—those that affect the exocrine cells in the pancreas and those that affect the endocrine cells. Exocrine cells are glands that secrete hormones and other substances through ducts in the body, whereas endocrine cells secrete hormones directly into the bloodstream. The pancreas has both types of cells.Exocrine Pancreatic Cancers
- Pancreatic adenocarcinoma: This is the most prevalent form of pancreatic cancer, accounting for about 90 percent of all diagnoses. It affects the exocrine cells in the pancreas ducts that produce digestive enzymes.
- Squamous cell carcinoma: This extremely rare cancer forms in the pancreatic ducts from squamous cells not naturally present in the pancreas. This type is so rare that there have not been enough reported cases for its origins to be wholly understood. Rarely discovered early, it has a very poor prognosis.
- Adenosquamous carcinoma: Accounting for 1 to 4 percent of exocrine pancreatic cancers, this rare pancreatic cancer presents elements of both ductal adenocarcinoma and squamous cell carcinoma. Compared to adenocarcinoma, adenosquamous carcinoma is more aggressive and has a poorer prognosis.
- Colloid carcinoma: Comprising only 1 to 3 percent of exocrine cases, this rare form typically develops from a particular type of benign cyst, an intraductal papillary mucinous neoplasm (IPMN). Because a pancreatic colloid tumor consists of malignant cells suspended in a gelatinous substance known as mucin, it spreads more slowly, is easier to treat than other pancreatic cancers, and has a much better prognosis.
Neuroendocrine Pancreatic Cancer
This type accounts for 5 percent of pancreatic cancer diagnoses. It starts in the endocrine cells, which produce hormones affecting many body processes from metabolism to blood sugar to mood. Survival and recovery rates for this type of cancer are better than those for adenocarcinoma.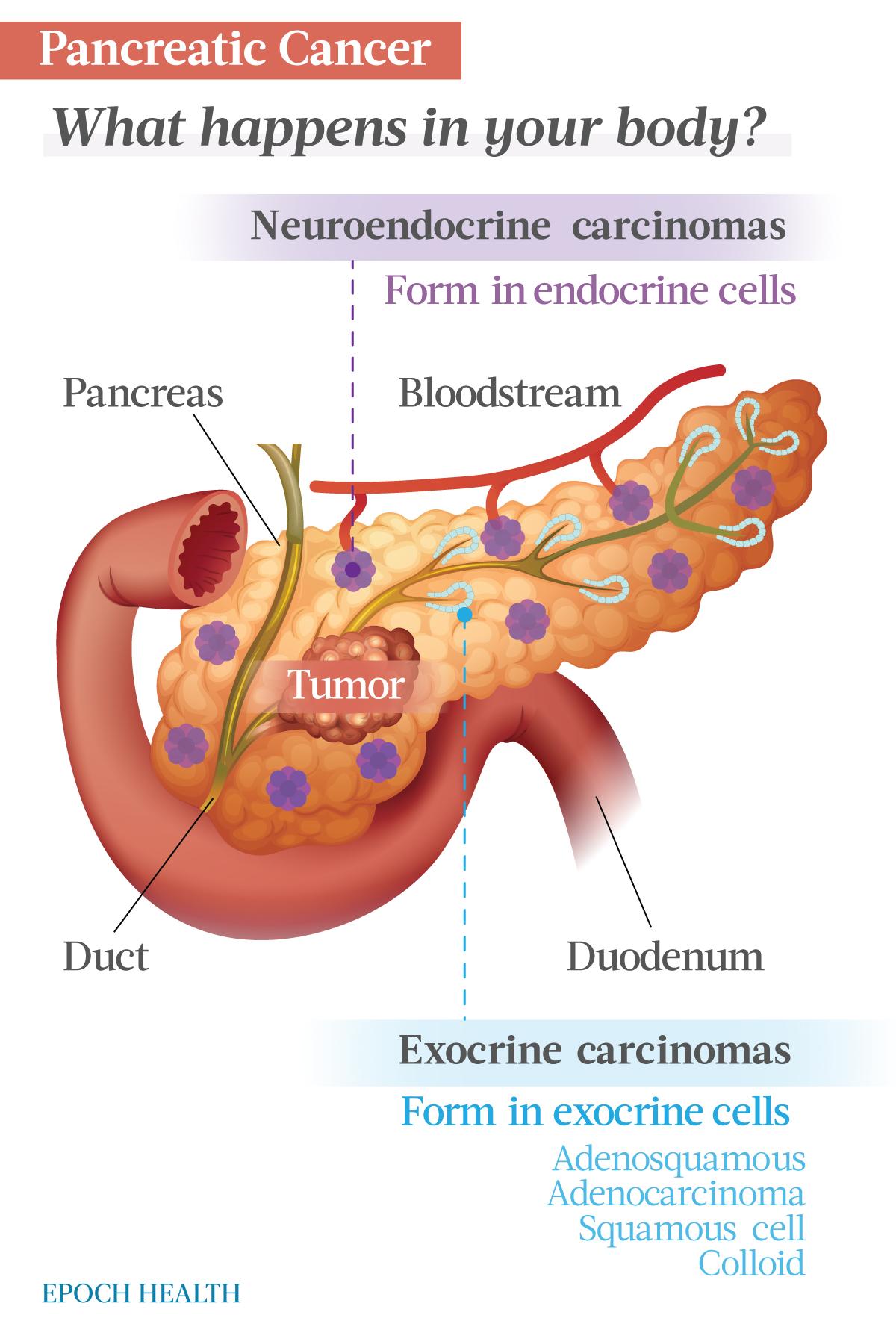
Benign Precancerous Lesions
Cysts and other benign tumors, including IPMNs, can form in the pancreas, and some can result in pancreatic cancer. IPMNs and other benign lesions are often discovered while a patient is being scanned for an unrelated condition. Depending on the type of growth and location, your doctor may recommend surgical removal of the lesion or continued monitoring.What Are the Symptoms and Early Signs of Pancreatic Cancer?
Pancreatic cancer typically doesn’t cause symptoms until it reaches advanced stages. Thus, reliable, early signs are hard to detect.- Loss of appetite
- Unplanned weight loss
- Abdominal pain that can radiate to the back
- Lower back pain
- Blood clots (often in the legs, which can manifest as redness, pain, and swelling)
- Jaundice
- Depression
- Light-colored or slimy stools
- Dark-colored urine
- Itchy skin
- Nausea and vomiting
- Sudden-onset diabetes or the exacerbation of preexisting diabetes
Despite the poor prognosis, pancreatic cancer is potentially curable if diagnosed early. According to Johns Hopkins Medicine, up to 10 percent of patients diagnosed early become disease-free posttreatment. The pancreatic cancer survival-time average is three to three-and-a-half years for patients diagnosed before the tumor grows or spreads.
What Causes Pancreatic Cancer?
Your pancreas is a gland in the abdomen, between the stomach and spine. It produces hormones that regulate blood sugar levels and enzymes that aid digestion. Pancreatic cancer occurs when the DNA in your pancreas cells develops mutations.A cell’s DNA contains the blueprints for cell development and death. Such cancerous mutations instruct cells to grow without limit and to persist after normal, healthy cells would perish. In some rare cases, these mutations can be inherited.
Who Is More Likely to Develop Pancreatic Cancer?
These factors are associated with an increased risk for pancreatic cancer:- Smoking and use of all forms of tobacco
- Obesity, particularly belly fat
- Excessive alcohol consumption
- Diabetes, especially type 2 diabetes. Sudden-onset diabetes can be a sign of pancreatic cancer.
- Chronic pancreatitis, inflammation of the pancreas
- Exposure to certain chemical toxins, such as pesticides and petrochemicals
- Family history of genetic vulnerability, such as BRCA1 or BRCA2 genes inherited from a parent
- Blood type other than O
What Are the Tests to Detect Pancreatic Cancer?
If a person exhibits symptoms associated with pancreatic cancer, specific tests and procedures will assist in diagnosis. If cancer is detected, follow-up tests will help assess the extent of the cancer.- Imaging tests: These diagnostic tools give doctors an image of your pancreas and surrounding organs. Techniques used include magnetic resonance imaging (MRI), ultrasound, computerized tomography (CT scan), and positron emission tomography (PET scan).
- Endoscopic ultrasound (EUS): A tube is passed down the esophagus to provide images from within the abdomen of the pancreas and other adjacent organs.
- Biopsy: A small sample of tissue is collected either through a tool inserted into the EUS or, more rarely, via a pin inserted into the pancreas via the abdomen.
- Blood test: This test looks for specific proteins in the blood shed by pancreatic cancer cells. The test looks for a particular marker, CA 19-9. This marker may help indicate how well you will respond to treatment. However, not all patients with pancreatic cancer test positive for these markers, so the test’s diagnostic power is limited.
- Genetic testing: If you are diagnosed with pancreatic cancer, consider getting genetic testing done. This can determine if there’s a hereditary susceptibility in your family to the condition. It can also help your doctors chart a course of treatment for you.
What Are the Complications of Pancreatic Cancer?
Pancreatic cancer can develop several complications, typically involving the organs of the digestive system and the nerves surrounding the pancreas.Bowel Obstruction
A pancreatic tumor can obstruct the duodenum (the initial passage of the small intestine), blocking the movement of digested food from the stomach into the intestine. In this case, your physician may recommend inserting a stent into your small intestine to keep it unobstructed. In some situations, you may need to undergo surgery to have a temporary feeding tube placed or to have the attachment of the stomach relocated to a lower point of the intestines not blocked by cancer.Jaundice
Pancreatic cancer can block the liver’s bile duct, causing jaundice. The signs of jaundice include yellow skin and eyes, pale stools, and dark urine. Your doctor may recommend inserting a stent (a plastic or metal tube) into the bile duct to keep it unobstructed.Pain
A growing tumor may impinge on nerves in your abdomen, resulting in pain that may become severe. Pain medications may be prescribed to manage this pain. In addition, radiation and chemotherapy treatments may slow tumor growth and relieve some pain.Weight Loss
Several aspects of pancreatic cancer can cause weight loss. Weight loss might occur as the cancer disrupts the body’s metabolism. Nausea and vomiting caused by treatments or a tumor putting pressure on the stomach may make eating solid food difficult or impossible. Also, the body may not be able to fully process food because the pancreas isn’t producing enough digestive juices.What Are the Treatments for Pancreatic Cancer?
Pancreatic cancer treatment depends upon the cancer’s stage and location and the patient’s overall health and personal preferences. Treatment can involve surgery, radiation, or chemotherapy. In late-stage cancer, treatment may focus on palliative (supportive) care.Surgery
Surgery aims to remove the cancerous tumor(s) from the organ. The procedure used will depend upon the location of the cancer in the pancreas.- Pancreaticoduodenectomy (“Whipple procedure”): This procedure is used when the cancer is in the head of the pancreas. The operation requires surgical skill to remove the head of the pancreas, the duodenum, the gallbladder, part of the bile duct, and adjacent lymph nodes. Sometimes part of the stomach and colon are removed as well. Then, the surgeon reattaches the remaining parts of these organs to allow the patient to digest food.
- Distal pancreatectomy: This procedure removes the pancreas’ left side (body and tail). The procedure may also involve removing your spleen.
- Total pancreatectomy: As the name implies, this procedure completely removes the pancreas. While you can live relatively normally without this organ, you will need lifelong insulin treatments and enzyme replacement therapy.
- Surgery for tumors affecting nearby blood vessels: If the tumor(s) involve nearby blood vessels, you may not be a candidate for the above surgical interventions. In that case, at some state-of-the-art medical centers, surgeons may offer operations that include removing and reconstructing the affected blood vessels.
Chemotherapy
Chemotherapy uses drugs that are toxic to cancer cells. The drugs are administered as pills or through an IV.Radiation Therapy
Radiation therapy directs high-energy X-rays at the tumor to kill cancer cells. It is typically combined with chemotherapy. It may also be used for advanced patients who are not eligible for surgery to ease symptoms.Targeted Therapy
In this treatment, drugs are used to target specific proteins that determine the spread and growth of the cancer. This therapy may also be combined with other modes of treatment. For example, erlotinib, olaparib, larotrectinib, and entrectinib are common medications for targeted therapy.Pain Management
Pancreatic cancer can involve nearby nerves, which can be very painful. Your doctor may prescribe oral medications, steroid injections, or nerve blocks to manage the pain.If you have pancreatic cancer, talk to your doctor to determine a treatment to ease your symptoms if you’ve started experiencing severe and enduring pain.
How Does Mindset Affect Pancreatic Cancer?
According to the American Cancer Society, research has not shown that attitude, mood, or mind-body therapies impact cancer survival rates. Some recent research challenges that assessment, pointing out that “studies of the placebo effect are revealing that our mindsets can even leverage endogenous opioid and neuroimmune pathways, thereby directly changing physiology and shaping objective markers of health. During cancer treatment, mindsets about the meaning of illness (e.g., whether it is a catastrophe, a manageable challenge, or an opportunity to make positive life changes) are important.”However, it is important to note that there is no medical evidence to conclude that the patient “brought cancer upon themselves” through negative thinking or due to a particular personality type.
Less controversial in the research is the recognition that interventions like biofeedback, meditation, support group attendance, therapy for depression, and visualization can help manage symptoms, discomfort, and the mental challenges associated with such a diagnosis.
What Are the Natural Approaches to Pancreatic Cancer?
There is limited peer-reviewed research on natural approaches to pancreatic cancer.How Can I Prevent Pancreatic Cancer?
There is no surefire method to prevent pancreatic cancer, but there are steps you can take to reduce your risk.- Quit smoking: Smoking cigarettes is believed to cause roughly 25 percent of pancreatic cancers. Nicotine impacts the secretion of the pancreas. Smoking can cause the carcinogen N-nitrite to enter the bile duct and then reflux into the pancreatic duct, thus inducing pancreatic cancer.
- Balanced diet: Eat a light, low-fat diet, emphasizing cereals, beans, fish, and shrimp, vegetables such as radishes and green vegetables like broccoli and cabbage, and fruits such as grapes, kiwis, figs, and so forth.
- Outdoor aerobic exercise: Engage in regular exercise such as walking, cycling, and swimming. Exercise promotes vitality and immunity and exercises bones and muscles, which supports optimal tissue and organ functioning. It also prevents cancer due to its ability to mobilize the immune system and enhance T-cell function. In July 2022, a research team at the New York University School of Medicine published a study in the international oncology journal Cancer Cell. Researchers found that in mice afflicted with pancreatic ductal adenocarcinoma, aerobic exercise slowed tumor growth.
- Regular physical checkups: Regular physical examination and screening improve the detection rate of early pancreatic cancer, enhancing one’s prognosis and allowing physicians to use the full spectrum of treatments, including surgery, which is crucial to the long-term survival of this disease.
- Self-protection at work: If you work in an environment where you are exposed to chemicals, take all necessary precautions to reduce exposure, including wearing masks, gloves, and, where applicable, hazard suits.
- Develop a healthy mood: Stress can lead to an impaired immune system as well as metabolic and endocrine dysfunction. Impairments in these systems create a more inviting environment for cancer to develop and aggressively advance.