Modern medicine has progressed in large part by waging war against germs—snuffing out microscopic disease-causing creatures before they kill us.
The 19th-century discovery that microorganisms are the cause of infectious disease—the leading cause of death at the time—led scientists to the consensus that “germs” posed a great danger to humanity, a stance that’s been woven into policy and ideology to this day. Public health advancements in the 20th century proved that controlling infectious outbreaks
extended life expectancy and reduced infant and maternal deaths.
It was an era heralded for great medical achievements.
Death rates rapidly declined—even before the introduction of penicillin and vaccines—as public sanitation and better hygiene in hospitals transformed public health.
Mass antibiotic production came in the 1940s, initially for wounded soldiers, then exploded into the public sphere. These new antimicrobial weapons cured millions of infections and saved many lives. However, antibiotics also came with consequences that are squeezing today’s health care on two sides: superbug infections and a rise in all diseases.
Good, Bad, and Usually Ugly
The microbial world is diverse. While it’s true that some microbes cause disease, saying that all of them are killers would be like calling all dogs killers because of a few.
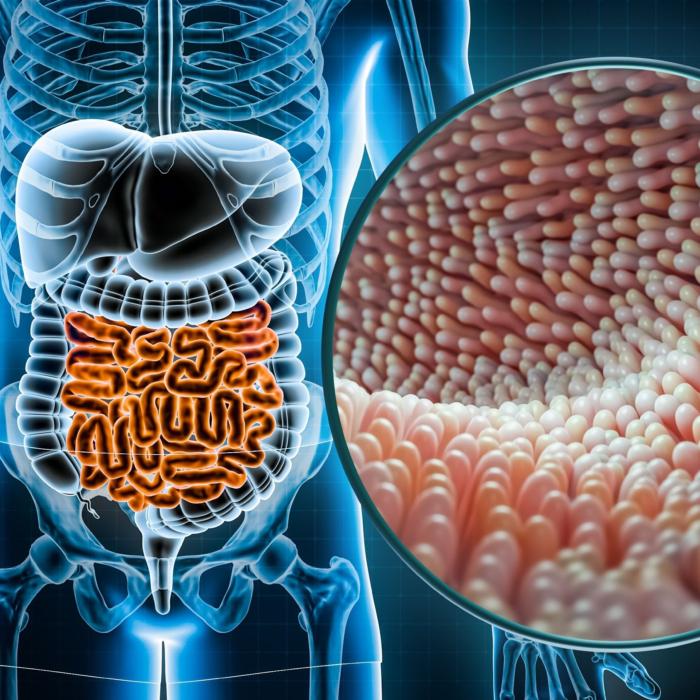
Researchers have learned that thinking of microbes as pathogenic, or disease-causing, is profoundly incorrect. In fact, the microbial world encompasses bacteria, viruses, and fungi that largely promote health. Human beings host a vast microbial community, or microbiome, which forms a kind of detached organ with interactions that keep us alive. These tiny creatures may not be cute, but they are essential.
“[There is] a consortium of organisms in us and on us and around us. There are trillions of them,”
Dr. Neil Stollman told fellow physicians at a recent Malibu Microbiome Meeting. “When we lose bugs, we are at risk of other bugs hurting us. They are intimately involved in our immune system development. And we help them. We provide a home for them and nutrients.”
Stollman is chairman of gastroenterology at Alta Bates Summit Medical Center in Oakland, California and past chairman of the American College of Gastroenterology.
Bugs Everywhere
Everyone has an individually unique microbiome, as well as distinct microbiomes in different areas of their bodies. We have microbes, for instance, on our skin and in our mouths, lungs, nasal passages, urinary tract, and especially in our gastrointestinal tract, and some of those microbes indeed are associated with illness.
One database offers 5,677 associations between 1,781 microbes and 542 human diseases across more than 20 sites on the body.
Not surprisingly, the gastrointestinal tract was associated with 37 percent of those disease associations, with the oral cavity next at less than 10 percent. However, that doesn’t mean researchers understand this realm all that thoroughly.
Dr. Sabine Hazan said more than 95 percent of microbes are still a mystery
. A gastroenterologist and researcher, she presented microbiome discoveries from the past four years at the Malibu Microbiome Meeting.
“We have no idea what their names are and what they do, and possibly, they could be the culprit of a disease,” Hazan said. That also means researchers don’t know the precise synergistic roles those microbes play in the body that keep us alive and healthy. This collection of microbes, or flora, remains largely a mystery though it is an area of intense interest to researchers.
Tiny Organisms With Big Jobs
Microbiome studies tend to focus heavily on the gut, where our microbes configure the majority of our immune system. High levels of certain beneficial bacteria help us
mount a robust response to invading viruses, for example. We know now that a diversity of flora is protective against disease.
Other processes that happen in the gut are critical to life, including metabolism, hormonal regulation, and neurological function. Various microbes throughout the gut
set off a chain of signals to cells that are involved in hormone release and metabolic processes such as insulin sensitivity, appetite, and fat storage. Metabolic disorders such as insulin resistance and diseases of the heart and circulatory system, as well as endocrine disorders that affect organs that rely on hormones, all lean on the microbiome.
Acceptance of the notion that the gut and mental health are connected has ebbed and flowed for decades, but metabolic processes instigated by bacteria can affect both the
permeability of the gut lining and
flip on inflammatory pathways. Both of these can affect mental health, as well as a plethora of other conditions and physiological systems, and now have wide acknowledgment.
Undoing a History of Hygiene
Historically, even as recently as the COVID-19 outbreak, medicine has been obsessed with pathogenic microbes, while commensal (helpful) bacteria haven’t gotten credit for the grunt work they do to keep us alive and healthy.
The problem is historical, in some sense. It goes back to our earliest concepts of the microbial world, when doctors including
Ignaz Semmelweis hypothesized in the 1840s that physicians and medical students were transmitting “death particles” from autopsy rooms where they started their workday to clinics where they delivered babies for the remainder of the day.
That gave rise to the practice of routine hand-washing, with immediate and observable effects. But by the time we learned that many microbes played beneficial roles, there were already massive industries built around the war against microbes. Food processing, chemically treated crops, and overreliance on pharmaceuticals destroyed massive volumes of health-sustaining microbes.
One result of this assault is the
seemingly unending dilemma of deadly superbugs that have become resistant to antibiotics. Allergies, asthma, autoimmune disorders, and inflammatory bowel diseases have all been linked to the oversterilization of our microbial environment. Killing microbes is a multibillion-dollar industry.
“Clearly, there are those who will want to defend the past and even the status quo. That is to be expected,”
Dr. David Perlmutter, neurologist and fellow of the American College of Nutrition, wrote in his book “
Brain Maker.” “I believe it is far more important to break the bonds of these constraints and recognize that our most exciting and respected science is offering us an incredible opportunity to regain our health through the force wielded by the microbiome.”
Cultivating Our Gut Microbiome to Stifle Disease
More from this series
Medicine’s Philosophical Shift
Medicine is confronted with a crossroads: keep on the current anti-microbial path or reset our medical paradigm around the reality that our various microbiomes help sustain us while also fighting off infection and disease.Many of the rapidly growing diseases we’re contending with today—such as autism and autoimmune disorders—have now been linked to microbiome health. A combination of lifestyle factors—from foods that feed the wrong microbes, to routine chemical exposures, and unnecessary antibiotics—have undoubtedly taken a toll on our symbiotic microbes and health, Hazan said.
“Have we in essence killed our microbiome? Could it be maybe we’re overdoing it?” she asked.
Concepts that include precision health and personalized nutrition hinge on a broad understanding of the gut microbiome, a race that has spurred investment in new companies with promises that have far outpaced the available research.
Scientists at the Malibu Microbiome Meeting shared absurd claims of products that insinuate one single probiotic can reverse specific diseases.
“To simply believe you’re going to take one pill of one particular bacteria and it’s going to solve your problem and provide some beautiful homeostasis to your microbial ecosystem is absurdly simplistic and is absolutely not true,” Stollman said.
And yet, there are also miraculous case studies indicating incredible promise. Trials are underway, at rapid rates. In fact, more than 80 percent of microbiome research has occurred since 2017, according to Stollman.
“There’s a real mania about the biome. I think the mania is also based not as much on ‘can we improve our health?’ but rather ‘can we diagnose an illness, and treat an illness?’” he said.
The challenge ahead is significant. Beyond fixing outdated medical protocols, like indiscriminate antibiotic use, there is the staggering volume of microbes and microbial interactions that need to be understood. Considering that our cells perform impossible complex chemistry at a scale and intricacy beyond anything modern science can match, imagine the additional complexity of trillions of microorganisms doing something similar.
Microbiome science may be new, but researchers have made undeniable connections between various bacteria and specific diseases. The truth of Hippocrates’s statement that “all disease begins in the gut” is starting to be recognized by today's scientists.