Yeast, specifically Candida albicans, is a fungus commonly found in the digestive system and on the skin and other body parts.
Under normal conditions, it coexists with us without causing problems. However, yeast infections, also known as candidiasis, occur when there’s an overgrowth of this fungus. Approximately 75 percent of adult women will develop at least one infection in their lifetime.
What Causes a Yeast Infection?
Candida comprises approximately 150 yeast species, with Candida albicans being responsible for about 70 percent to 80 percent of all candidal infections.
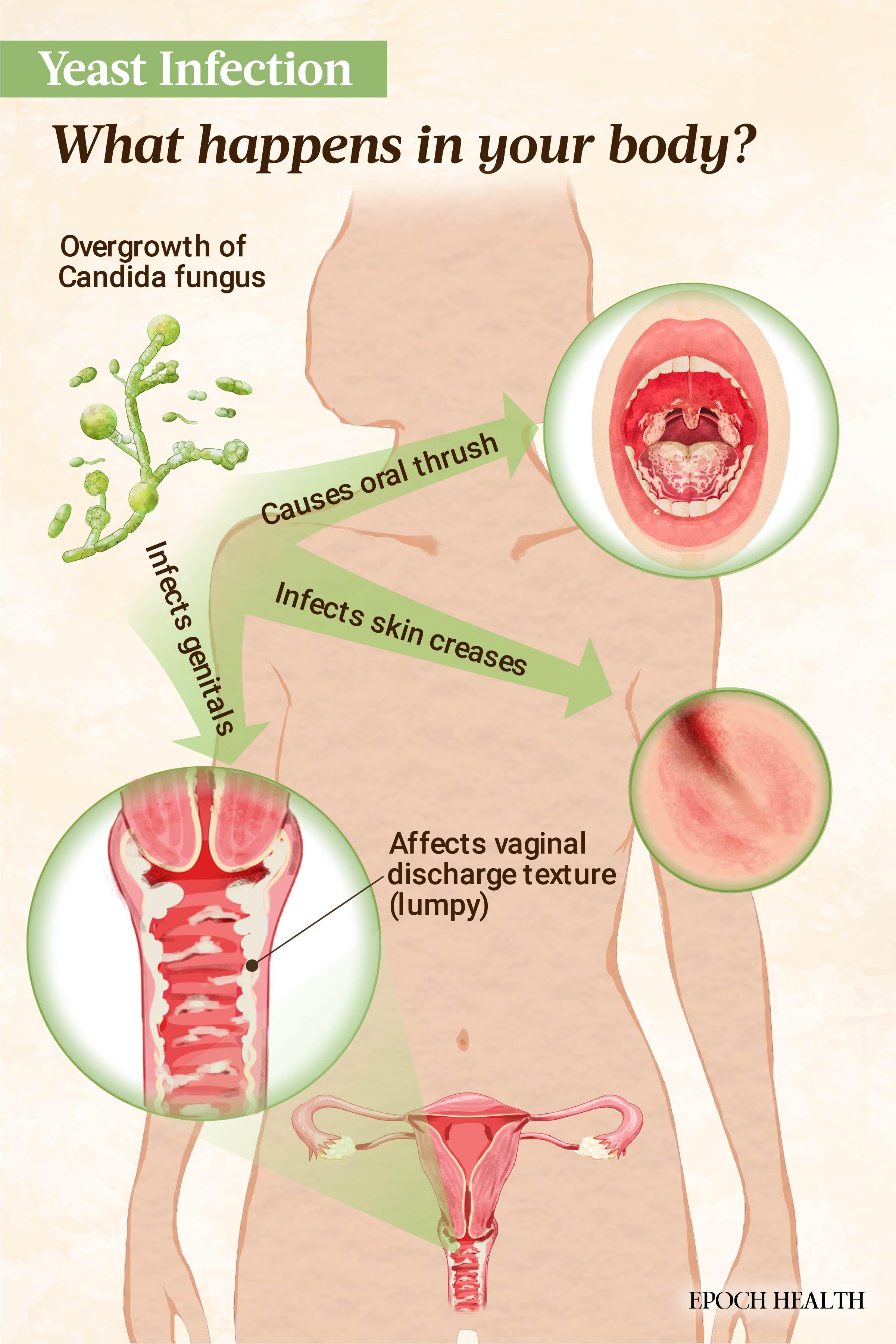
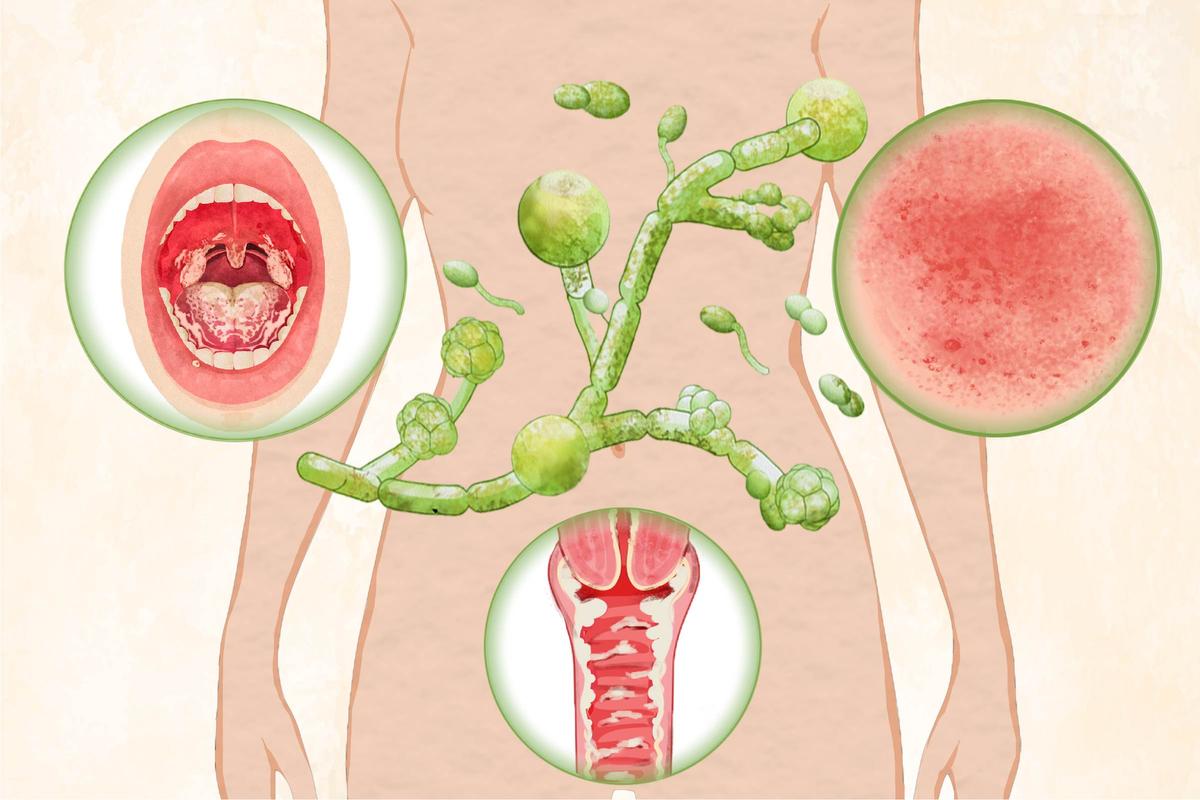
Most yeast infections are caused by an overgrowth of the fungus Candida albicans. Infections can affect the mouth, skin folds, genitals, or, in severe cases, the bloodstream. (Illustration by The Epoch Times, Shutterstock)
What Are the Types of Yeast Infections?
There are many types of yeast infection, with the main types being:
- Vaginal: Vulvovaginal candidiasis is the most common type of yeast infection. It is not a sexually transmitted disease (STD) or infection (STI).
- Penile: Penile candidiasis is located in and around the penis.
- Skin: Yeast infections can occur on the skin (cutaneous candidiasis), especially in warm and moist areas such as skin folds, under the breasts, in the navel, or in the groin area.
- Diaper rash: Yeast diaper rash is known as candidal diaper dermatitis or diaper candidiasis, a subtype of yeast skin infection.
- Oral thrush: Oral thrush, also known as oral candidiasis, affects the mouth. Candidiasis in the mouth and throat is known as oropharyngeal candidiasis. When Candida affects the esophagus, it’s called esophageal candidiasis or Candida esophagitis.
- Invasive candidiasis: Different from the other types, invasive candidiasis is a severe infection that can impact various organs and systems in the body, including the blood, heart, brain, eyes, and bones. It tends to affect immunocompromised individuals and is on the rise due to advanced invasive medical technology. When Candida enters the bloodstream or internal organs (for instance, from the skin surface), it’s called candidemia. Candidemia is the main cause of invasive candidiasis and is the most frequent cause of bloodstream infections among hospitalized patients in the United States. The most common species causing invasive candidiasis is Candida albicans.
What Are the Symptoms and Early Signs of a Yeast Infection?
The signs and symptoms of yeast infection vary based on the type. They are grouped below as such:
Vaginal
An estimated 20 percent of women with vaginal candidiasis don’t experience any symptoms. Symptoms are usually mild, and they may intensify a few days prior to the onset of your period. Symptoms include:- Itchy, sore, or burning vagina
- Discomfort or pain during sex
- Painful or uncomfortable urination
- Abnormal white or yellowish vaginal discharge (e.g., cottage cheese-like white discharge or watery discharge). However, it doesn’t have a bad smell. (A bad smell may indicate a different kind of infection.)
- Inflammation and redness around the vulva
- Swelling around the vulva
- Fissures in the vaginal wall
Penile
Common symptoms include:- Redness, scaling, and a painful rash on the underside of the penis
- A red rash under the foreskin
- Small red spots on the glans (tip of the penis)
- Penile discharge
- Pain during urination and difficulty retracting the foreskin
- A yeasty-smelling “cheese-like” substance under the foreskin
Skin
Common symptoms of a skin yeast infection include:- Red and expanding rash with skin breakdown
- Rash in skin folds (e.g., belly area, buttocks, under breasts, armpits, and other areas)
- Fluid-filled patches
- Hair follicle infection resembling pimples
- Intense itching or burning sensation
Diaper Rash
Among infants, Candida albicans is the main culprit in diaper rash, which thrives in the warm, moist environment of diapers. Infants with Candida diaper dermatitis often show Candida colonization in their gastrointestinal tract. Candidal colonization in the rectum and stools is found in 21 percent to 62.5 percent of very low birth weight infants (≤ 3.3 pounds). Symptoms of diaper candidiasis may include:- Deep red skin color with patches outside the diaper region
- Possible mouth thrush occurring at the same time
- Rash affecting the creases or folds of the thighs and diaper area
Oral Thrush
Symptoms of oral thrush may include:- White patches (plaques) inside the cheeks, tongue, roof of the mouth, and throat. They can be wiped off, revealing red areas that may bleed slightly.
- Redness in the mouth and throat.
- Feeling like cotton in the mouth.
- Pain during eating or swallowing.
- Redness and cracks at the mouth corners.
- Reduced sense of taste or an unpleasant taste in the mouth.
- Difficulty swallowing.
- Pain when swallowing: This is the distinctive feature of esophageal candidiasis.
- Chest pain behind the breastbone.
- Abdominal pain.
- Heartburn.
- Weight loss.
- Diarrhea.
- Nausea and vomiting.
- Dark black stool (melena).
Invasive Candidiasis
Invasive candidiasis symptoms can be challenging to determine, as most patients with this type of infection already have other illnesses. However, fever and persistent chills, unaffected by antibiotic treatment, are typical signs of invasive candidiasis.Who Is at Risk of a Yeast Infection?
Anyone can develop a yeast infection, but the following factors increase one’s risk:
- Skin damage.
- Poor hygiene.
- Warm or humid environments: Not changing diapers or undergarments often enough in children and older adults can cause diaper candidiasis, as wet diapers can cause yeast to grow excessively. In addition, wearing wet clothes for a long time can exacerbate an infection.
- Weakened immune system: Weakened immunity due to HIV infection, chemotherapy, or organ transplantation raises risk.
- Antibiotics: Antibiotics disrupt normal bacterial flora, creating an environment that promotes the growth of potential pathogens such as Candida. Oral thrush often occurs with antibiotic use, although only a small percentage of antibiotic users develop it. Around one-quarter to one-third of women are susceptible to vaginal candidiasis while taking or after completing broad-spectrum antibiotics.
- High sugar levels: Sugar serves as nourishment for the yeast fungus, promoting its growth.
- Hormonal changes: Increased estrogen levels during pregnancy can alter the balance of microorganisms and raise the risk of a vaginal yeast infection. Contraceptive pills also affect a woman’s hormone levels similarly to pregnancy, as do menstrual cycle changes.
- Partner contact: Though not considered an STI, people can sometimes contract a yeast infection from someone else during sexual contact. For instance, a man with an excessive amount of the infection on the head of the penis can pass the infection on to his partner. Sexual contact with an infected partner may lead to symptoms such as itching, rash, or irritation. It’s advisable for your partner to consult a doctor and use antifungal medication if needed to avoid the “ping pong effect,” a cycle of infection and reinfection via partner contact that sometimes occurs in cases of recurring infections.
- Change in the skin’s pH balance.
- Diabetes.
- Corticosteroids (including inhaled corticosteroids).
- Sex: Women of childbearing age, especially those between the ages of 20 and 40, are most susceptible. Vaginal sponges, diaphragms, and intrauterine devices (IUDs) may raise the risk of yeast infections. Spermicides generally do not cause yeast infections but may lead to vaginal or vulvar irritation in some women, so in this way, they may increase susceptibility. Related skin conditions that affect the vulva, such as eczema and psoriasis, also increase risk.
- Obesity: Individuals with large skin creases or folds are prone to developing skin yeast infections.
- Clothing or pads: Synthetic and tight-fitting clothing (e.g., underwear, yoga pants) and nonbreathable panty liners, sanitary pads, or incontinence pads raise a person’s risk.
- Stress: People under stress or suffering from lack of sleep are more prone to infections.
- Circumcision: Uncircumcised men are typically more at risk of yeast infections than circumcised.
- Infants: Vaginal yeast infections can be transmitted to babies during childbirth, potentially causing diaper rash. Babies taking antibiotics or whose mothers are on antibiotics while breastfeeding are more susceptible.
- Smoking: Smoking increases the risk of oral thrush.
- Iron or vitamin B12 deficiency: This deficiency makes one more susceptible to oral thrush.
- Hypothyroidism: People with an underactive thyroid are more at risk.
- Dentures, especially when they are ill-fitting.
How Is a Yeast Infection Diagnosed?
Your doctor will inquire about your symptoms and medical background, conduct a physical examination, and may take a skin or nail sample for diagnosis confirmation, if applicable. A pelvic exam may reveal swelling and redness of the skin in the vulva, vagina, and cervix, dry white spots on the vaginal wall, and cracks in the skin of the vulva in a suspected vaginal yeast infection. Sometimes, your doctor may request additional tests to investigate other potential causes of your symptoms.
Diagnostic tests may include:
- Wet mount: A wet mount is commonly used to examine vaginal discharge under a microscope. A sample of the discharge is taken with a cotton swab.
- KOH test: Your doctor collects a sample from the infected area by scraping it lightly. The sample is then placed on a slide with potassium hydroxide (KOH) solution and gently heated and observed for three to five minutes for a reaction. This solution dissolves skin cells but not the fungus, allowing the fungus to be observed under a microscope.
- Swab test: Genital candidiasis can be diagnosed by a genital exam by your doctor, and confirmation may be obtained through a swab test, which involves collecting a sample from the affected area for lab testing, confirming if Candida is the cause and eliminating other possibilities.
- Endoscopy: This involves using a tube equipped with a light and camera to inspect the digestive tract and can confirm an esophageal candidiasis diagnosis.
- Biopsy: For esophageal candidiasis, your doctor may perform a biopsy by taking samples from the plaques on the esophageal mucosa for testing.
- Blood sample: Doctors typically diagnose invasive candidiasis by culturing a blood sample or a sample from the infected area to check for Candida growth in a lab.
What Are the Complications of a Yeast Infection?
Aside from invasive candidiasis, yeast infections typically do not result in serious health complications but may recur frequently. The following are complications that may occur, depending on the type of infection:
- Vaginal: Serious complications from yeast infections are rare and typically occur in individuals with weakened immune systems. In such cases, inflammation may escalate and extend to other areas. Excessive scratching can also lead to skin cracking, increasing the risk of a skin infection. Vaginal infections during pregnancy can slightly increase the risk of birth complications such as premature labor, miscarriage, or preterm birth. Approximately 5 percent to 9 percent of women experience recurrent yeast infections, characterized by three or more confirmed infections within a year.
- Penile: Common complications include balanitis, scarring and constriction of the penis, and impaired blood flow to the penile tip.
- Diaper rash: Granuloma gluteale infantum is a reaction to a prolonged Candida diaper rash that leads to reddish bumps or persistent lumps on the skin in the diaper area.
- Oral thrush: Difficulty swallowing, respiratory distress, and infections spreading throughout the body are possible complications. Progression to candidal esophagitis is a concern for people with HIV/AIDS. Complications of esophageal candidiasis include esophageal ulcers that can rupture, upper gastrointestinal bleeding, weight loss, malnutrition, sepsis, and narrowing of the esophagus.
- Invasive candidiasis: Invasive candidiasis can have serious complications, such as cerebral microabscesses, which are collections of pus and infected tissue within the brain. It can also lead to endocarditis, an infection and inflammation affecting the inner lining of the heart, ophthalmologic complications, and death.
What Are the Treatments for a Yeast Infection?
In most cases, symptoms resolve completely with appropriate treatment. One reason most vaginal yeast infections resolve on their own is that women’s vaginal pH balance naturally becomes more acidic during the menstrual cycle, creating an inhospitable environment for yeast cells, leading to their natural decline. When treatment is needed, the following are possible options.
Antifungals and Other Medications
If the candidiasis is mild, typically, one treatment course suffices. The following are types of antifungal treatments and other pharmaceuticals:- Over-the-counter (OTC) antifungal medication, including ointments, creams, and medicated suppositories. Certain infections due to Candida species other than Candida albicans are resistant to OTC antifungal treatments. Some antifungal medications are oily, which can increase the porosity of contraceptives such as condoms, potentially allowing sperm to pass through them. In addition, pregnant women shouldn’t use OTC medications. Girls under 12 should consult their doctors before using them.
- Single dose of oral fluconazole: This medication’s mild side effects may include stomach upset, headache, and rash. It is not recommended for pregnant women.
- Other medicines: These include tioconazole, butoconazole, flucytosine, boric acid, and ciclopirox. The duration of treatment will vary from one to seven days. Completing the prescribed medication course in its entirety is crucial to avoid recurrence. Miconazole, nystatin, or clotrimazole may be used for penile candidiasis. Common medicines for skin infections include miconazole, clotrimazole, oxiconazole, ketoconazole, econazole, ciclopirox, and nystatin. Typically, skin yeast infections start to clear up within a week of treatment, but you must complete the prescribed medication course. Nystatin ointment or powder is often used for diaper rash and has a clinical cure rate of around 85 percent.
- -Azole creams: In the case of recurring vaginal yeast infections, “-azole” creams (such as clotrimazole) may be used once a week.
- Echinocandin medication: Treatments for invasive candidiasis depend on the patient’s age, infection location, and severity. For most adults, the first-line treatment is an echinocandin medication administered intravenously, such as caspofungin, micafungin, or anidulafungin. In specific cases, fluconazole, amphotericin B, or other antifungal drugs may be used.
Hygiene
Proper hygiene practices are also important in resolving yeast infections.A woman’s vagina maintains cleanliness on its own, so the use of products such as douche and feminine sprays is unnecessary. To treat vaginal discharge, you can do the following:
- Keep your genital area clean and dry by avoiding soap and using water only.
- Sit in a warm (not hot) bath, which may alleviate symptoms.
- Avoid bubble baths, as these can alter the vaginal pH and irritate sensitive areas.
- Avoid douching, as it can worsen vaginal discharge by removing healthy bacteria that protect against infection.
- Refrain from using feminine hygiene sprays, deodorant tampons, fragrances, or powders in the genital area.
- Avoid tight-fitting pants or shorts to prevent irritation and sweating.
- Avoid using scented toilet paper and scented menstrual products.
- Change menstrual products frequently during your period.
- Opt for cotton underwear or cotton-crotch pantyhose over silk or nylon to reduce moisture and yeast growth.
- Maintain good blood sugar control if you have diabetes.
- Do not wear wet bathing suits or exercise clothing for prolonged periods. Take them off immediately after you finish swimming or exercising, and wash sweaty or wet clothes after each use.
- Possibly switch laundry detergent and avoid fabric softeners.
- Abstain from sex: Repeated painful intercourse during candidiasis episodes can cause persistent vaginal and vulval pain, even after treatment. Therefore, it may be advisable to abstain from sex during these periods.
- Avoid sharing towels with others.
- Wear loose-fitting underwear, such as boxers.
How Does Mindset Affect a Yeast Infection?
A positive mindset can influence yeast infections in various ways.
As mentioned earlier, stress is a risk factor for Candida infections, such as recurrent vaginal candidiasis. A positive mindset encourages healthy coping strategies, such as mindfulness and gratitude, which can then contribute to lower stress levels and better overall mental health.
Positivity also fosters emotional well-being, which may contribute to a stronger immune response, thus helping the body fight off yeast infections.
Additionally, having a positive mindset can lead to better self-care practices, such as maintaining good hygiene and following a balanced diet, which can both contribute to preventing and treating yeast infections.
What Are the Natural Approaches to a Yeast Infection?
Several natural remedies may offer relief for some people, but they may not be suitable or effective for everyone. Research is still needed, so consult your doctor before using any of them.
1. Herbal Medicine
Many herbs have antifungal and anti-inflammatory properties, and some can be used to inhibit Candida, including:- Garlic (Allium sativum): One 2023 study discovered that pure garlic demonstrated significant effectiveness against lab-cultured Candida albicans. Garlic oil was also discovered to have an inhibitory effect on Candida albicans cells, particularly by influencing important genes related to energy production, cell growth, and protein processing. In addition, allicin, one of garlic’s main active compounds, can protect against Candida albicans overgrowth and reduce the risk of the fungus sticking to mouth cells.
- Roselle (Hibiscus sabdariffa): Roselle is known for various health benefits, such as lowering blood pressure, reducing inflammation, and fighting infections. Candida species can create stubborn infections by forming biofilms on mucosal linings and medical devices. One 2014 study found that roselle extract stopped Candida albicans from forming biofilms in lab tests, which is also important for fighting off recurring urinary tract infections. Another 2021 cell culture study discovered that roselle extract could even inhibit the growth of fluconazole-resistant Candida albicans.
- Holy basil (Ocimum sanctum or Tulsi): A 2022 systematic review of laboratory cell studies found that holy basil has strong anti-candidal properties likely due to its compounds such as eugenol and linalool. These make it a potentially useful addition to standard treatments for candidal infections.
- Chinese medicinal herbs: The extracts of various medicinal herbs, including Cortex Moutan (root bark of tree peony), Cortex Pseudolaricis (root bark of golden larch), rhizoma Alpiniae officinarum (rhizome of lesser galangal), rhizoma Coptidis, clove, cinnamon, Anemarrhena cortex phellodendri, Ramulus Cinnamomi, and Chinese gall, have demonstrated antifungal effects when applied directly to Candida species in lab tests.
- Cao Huang Gui Xiang (CHGX) formula: A 2022 study showed that the herbal formula Cao Huang Gui Xiang, which consists of Chinese licorice, ornamental rhubarb, the bark of Neolitsea cassia, and Pogostemon cablin, possesses potent antifungal activities against Candida species in lab tests.
2. Essential Oils
- Tea tree: Tea tree oil is an essential oil derived from the leaves of the tea tree plant (Melaleuca alternifolia) and is known for its antimicrobial properties. It has been widely used as a home remedy by some women with vaginal candidiasis. One 2004 study found that tea tree oil and its components, when used at concentrations between 0.25 and 1 percent, can work against Candida albicans cells by affecting their permeability and their membranes’ fluidity, thus negatively affecting these cells’ functions.
- Oregano: Essential oil derived from the leaves of the oregano plant (Origanum vulgare) possesses antiviral and antifungal properties. In one 2021 lab study, the seven most frequently used essential oils were tested against 10 Candida isolates, and direct application of oregano oil was found to be the most effective, as it could stop the attachment and formation of Candida biofilms.
- Other: A 2019 in vitro study found that the essential oils of several medicinal plants from Saudi Arabia, including Hart’s pennyroyal (Mentha cervina), basil (Ocimum basilicum), rue (Ruta graveolens), and pennyroyal (Mentha pulegium) are highly inhibitory on Candida species.
3. Lactoferrin
Lactoferrin is an important protein in our immune system and is considered a safe food additive. Due to its pharmaceutical and nutritional value, it is classified as a nutraceutical protein. In lab studies, human lactoferrin has been found to inhibit the growth of Candida albicans, binding to the fungus’ membrane and triggering an apoptosis-like cell death.It also works well with fluconazole against different Candida species, including some that are resistant to fluconazole. One 2008 study also found that a cream with lactoferrin could treat acute vaginal candidiasis.
4. Apple Cider Vinegar
In a 2018 in vitro experimental study, apple cider vinegar demonstrated inhibitory and fungicidal properties against Candida species. In one case published in 2019, a 32-year-old woman had been suffering from chronic vaginal candidiasis for the past five years, and she had tried several antifungal regimens to no avail. Her doctor later advised her to use a vaginal douche containing a mixture of water and apple cider vinegar twice daily. She didn’t receive any medical therapy during the treatment. After four months, her symptoms completely disappeared, and she remained free of vaginal candidiasis for two years (when the case report was published). It was not noted how long or how often the vinegar was applied.However, vinegar in any form can greatly irritate the vagina due to its extreme acidity. Therefore, it must be diluted and used with caution.
5. Baking Soda
Baking soda (Sodium bicarbonate), in a concentration of 0.5 percent or higher, can effectively reduce Candida albicans. In addition to having low abrasiveness, it is cost-effective and safe if swallowed accidentally. In one 2021 study, an experimental gel containing 5 percent sodium bicarbonate, 1 percent carbomer, and 94 percent water, was found to be highly effective against several common Candida species causing vaginal yeast infections. This gel is considered suitable for short-term use and shows promise for treating vaginal candidiasis effectively.6. Honey and Yogurt
One 2012 study compared women using a mixture of yogurt and bee honey applied vaginally to those using standard antifungal treatments for vaginal candidiasis. While clinical symptoms were better during the study with honey yogurt, the actual elimination of Candida was not as effective as the medication group. The researchers concluded that this mixture could be a helpful alternative or addition to antifungal treatments, especially for pregnant mothers. Greek yogurt with no added sugar, fruits, or flavor is recommended.How Can I Prevent a Yeast Infection?
You can minimize your risk of developing a yeast infection by practicing the following:
- Consume a variety of wholesome foods such as fruits, vegetables, whole grains, and lean proteins.
- Avoid unnecessary use of antibiotics.
- Avoid a high-sugar diet.
- Take antifungal drugs or antimycotics if you have weakened immunity.
- Manage other health conditions, such as diabetes.
- Take probiotics: For women experiencing frequent vaginal yeast infections, probiotics, such as yogurt with live cultures or Lactobacillus acidophilus tablets, may be beneficial. Lactobacilli may not only support the proliferation of beneficial bacteria but also help maintain a balanced local immunity.
- Wipe from front to back after using the restroom to prevent the spread of Candida albicans from the anus to the genitals.
- If you’re an uncircumcised man, ensure thorough cleaning beneath the foreskin.
- Practice safe sex and avoid engaging in sex with a partner who has a genital yeast infection.
- Ensure dryness in skin-on-skin areas and minimize friction. Always cleanse between fresh applications of drying powder.
- Maintain good oral hygiene: Rinse your mouth or brush your teeth after using inhaled corticosteroids and after meals. Brush your teeth twice daily and floss regularly.
- Avoid smoking.
- Regularly sterilize pacifiers, milk bottles, and toys to prevent babies from developing infections.